|



|
Synonyms: proximal tibial fracture, proximal tibia fracture
Tibial Plateau Fracture ICD-10
Tibial Plateau Fracture ICD-9
- 823.00 (closed upper end tibia fx)
- 823.02(upper end, closed, fibula with tibia
- 823.10(upper end, open tibia alone)
- 823.11(uppen end, open fibula alone)
- 823.80(fx unspecified closed tibia alone)
- 823.90(fx unspecified open tibia alone)
Tibial Plateau Fracture Etiology / Epidemiology / Natural History
- High-energy (MVA, Falls from height) in young patients, fragility fracture in elderly patients, periprosthetic fracture.
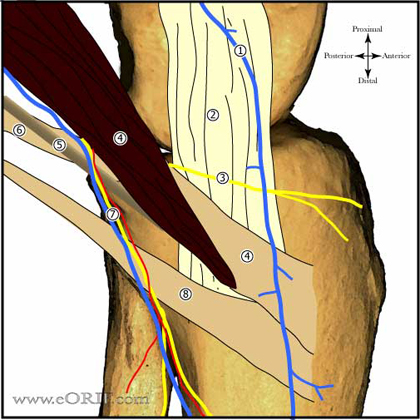
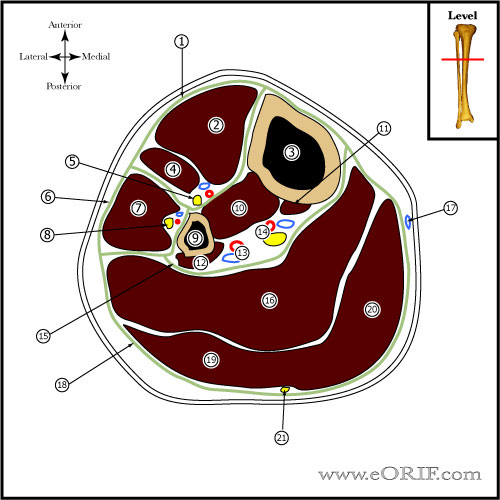
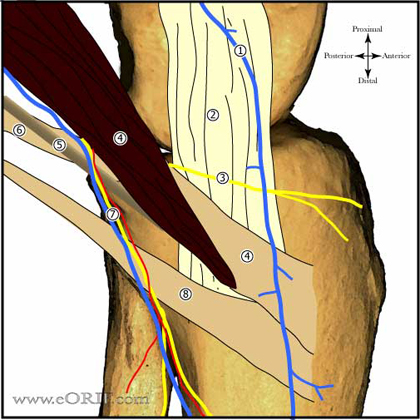
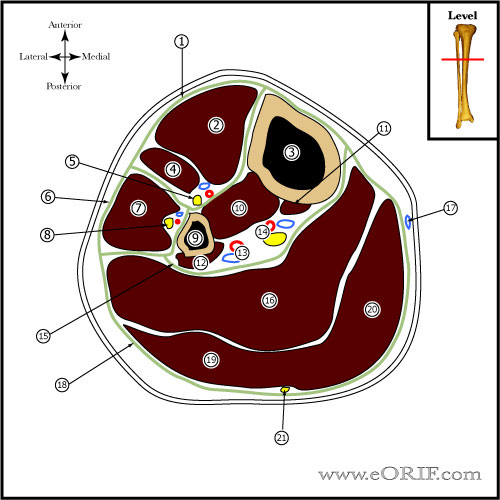
Tibial Plateau Anatomy
- Contact pressure elevation is seen when articular incongruity is >3mm: <1.5mm shows no significant increase in contact pressure. (Brown, J Orthop Res 6:851, 1988).
Tibial Plateau Clinical Evaluation
- Knee pain following trauma. Inability to ambulate, tenderness over site of injury.
- Hemarthrosis.
- Evaluate soft tissue injury. Auperficial abrasion / deep contusion / hemorrhagic blisters / massive swelling / skin wrinkles.
- Document neurovascular exam. Ankle-Brachial index <0.9 indicates need for Vascular Surgery consultation. ABI=systolic blood pressure palpated over the posterior tibial artery divied by SBP over the brachial artery at the elbow. Normal >0.9.
- Evaluate for compartment syndrome. Pain out of proportion or on passive stretch of the toes indicates need for compartment pressure monitoring. Monitoring is also indicated for an unconscious patient.
Tibial Plateau Xray / Diagnostic Tests
- A\P, lateral, internal/external oblique, 15 degree caudal tilt view. The degree of articular step-off is determined on the 15 degree caudal tilt view. Consider traction views for severe injuries.
- Increase in width of 1mm of medial or lateral clears space is suggestive of collateral ligament injury during stress views. Compare to opposite leg.
- CT scans with 2mm cuts and axial, coronal and sagittal reconstructions best identifies fx configuration. Best done in traction.
- Consider MRI to evaluate for associated meniscal and ligmanet injury (Yacoubian SV, JOT 2002;16:632).
Tibial Plateau Classification/Treatment
- Schatzker Classification (Schatzker, CORR 138:94, 1979
- Type I,-“pure cleavage”, split lateral plateau; generally younger pts, high risk of ligament injury (MCL), or trapped meniscus
- Nondisplaced (<2mm): Non-weighted bearing in knee immobilizer or cylinder cast for 7/10 days. Repeat films at follow-up, if stable switch to hinged- knee brace with toe touch weight-bearing x 8-12wks and isometric quad exercises with progressive passive/active assist ROM. (Segal D, CORR 1993;294:232) (DeCoster TA, CORR 1988;231:196)
- Displaced (>2mm, >10 degree angulation): ORIF vs CRPP, generally ligamentotaxis reduction and fixation with 6.5 or 7.0mm cancellous lag screws. Treatment is depended on the condition of the soft tissues. Consider spanning external fixation with delayed ORIF when soft-tissues permit for severe soft-tissue injury.
- Type II-“cleavage with depression”, split depressed lateral plateau fx
- Nondisplaced (<2mm):
- Displaced (>2mm, >10 degree angulation): ORIF. Generally ligamentotaxis reduction with depressed area elevated with bone tamps and packed with graft through fracture site or cortical window and fixation with peri-articular plate with multiple 3.5mm subchondral cortical "raft" screws proximally (Mills WJ, Orthop Clin North AAM 2002;33:177). Treatment is depended on the condition of the soft tissues. Consider spanning external fixation with delayed ORIF when soft-tissue permit for severe soft-tissue injury. Consider calcium phosphate cement augmentation of depressed segment (Trenholm A, JOT 2005;19:698).
- Type III-“pure central depression” of lateral plateau, lateral cortex intact; older pt, low risk of ligament injury
- Nondisplaced (<2mm): Non-weighted bearing in knee immobilizer or cylinder cast for 7/10 days. Repeat films at follow-up, if stable switch to hinged- knee brace with toe touch weight-bearing x 8-12wks and isometric quad exercises with progressive passive/active assist ROM. (DeCoster TA, CORR 1988;231:196)
- Displaced (>2mm, >10 degree angulation): ORIF. Depressed area elevated with bone tamps and packed with graft through fracture site or cortical window and fixation with 6.5 or 7.0mm cancellous lag screws. Treatment is depended on the condition of the soft tissues. Consider spanning external fixation with delayed ORIF when soft-tissues permit for severe soft-tissue injury.
- Type IV-medial plateau fx; high-energy, associated with traction injury to peroneal nerve
- Nondisplaced (<2mm):Non-weighted bearing in knee immobilizer or cylinder cast for 7/10 days. Repeat films at follow-up, if stable switch to hinged- knee brace with toe touch weight-bearing x 8-12wks and isometric quad exercises with early ROM. (DeCoster TA, CORR 1988;231:196)
- Displaced (>2mm, >10 degree angulation): ORIF. Generally ligamentotaxis reduction and fixation with peri-articular plate with multiple 3.5mm subchondral cortical screws proximally. Incisions determined by pre-operative CT. Plae should be placed with base over the apex of the fracture. Treatment is depended on the condition of the soft tissues. Consider spanning external fixation with delayed ORIF when soft-tissue permit for severe soft-tissue injury.
- Type V-Bicondylar. ORIF. Generally ligamentotaxis reduction fixation with lateral peri-articular locking plate with multiple 3.5mm subchondral cortical screws proximally. Consider separate medial incision and plating. Treatment is depended on the condition of the soft tissues. Consider spanning external fixation with delayed ORIF when soft-tissue permit for severe soft-tissue injury.
- Type VI-plateau fractures with dissociation of metaphysis and diaphysis. ORIF. Generally ligamentotaxis reduction fixation with lateral peri-articular locking plate with multiple 3.5mm subchondral cortical screws proximally. Consider separate medial incision and plating. Treatment is depended on the condition of the soft tissues. Consider spanning external fixation with delayed ORIF when soft-tissue permit for severe soft-tissue injury.
- Low Energy vs High Energy determined by (1)degree of articular depression, (2) extent and separation of the condylar fracture lines, (3)diaphyseal-metaphyseal comminution and dissociation, (4)integrity of soft tissue envelope
- With Distal femur fracture: high energy in injury. Consider temporary spanning external fixation with delayed ORIF. Parekh AA, J Trauma. 2008 Mar;64:736).
- AO Classification
- CPT: 27535(ORIF unicondylar)
Tibial Plateau Fx Associated Injuries / Differential Diagnosis
Tibial Plateau Fx Complications
- Stiffness
- Infection(up to 12%)
- Malunion
- Loss of fixation
- Skin loss
- Amputation
- Extensile exposures in tenous soft tissue can lead to complication rates as high as 50%
- Post-traumatic arthritis
- Painful Hardware
- Peroneal nerve palsy
- DVT/PE
Tibial Plateau Fx Follow up care
- Generally non-weight bearing for 3 months
Tibial Plateau References
- Watson, JT: High-Energy Fractures of the tibial plateau. Orthopedic Clinics North Am. 25:723-752, 1994
- DeBoeck and Opdecam, Posteromedial tibial plateau fractures: operative treatment by posterior approach. CORR, (320):125�128, 1995.
- Wyrsch B, McFerran MA, McAndrew M, et al: Operative treatment of fractures of the tibial plafond: A randomized, prospective study. J Bone Joint Surg 1996;78A:1646-1657.
- DeBoeck and Opdecam, Posteromedial tibial plateau fractures: operative treatment by posterior approach, CORR, 320: 125-128, 1995.
Georgiadis, Combined anterior and posterior approaches for complex tibial plateau fractures, JBJS Br, 76(2): 285-289, 1994.
- Rockwood and Green's Fractures in Adults: 2009
|