|


|
synonyms: rotator cuff tear, RTC tear, RC tear, RCT, RTC rupture
RTC Tear ICD-10
RTC Tear ICD-9
- 727.61 (non-traumatic complete rupture of rotator cuff),
- 726.10 (disorder shoulder tendon cuff)
- 840.3 (sprain and strain: infraspinatus)
- 840.4 (sprain and strain: rotator cuff)
- 840.5 (sprain and strain: subscapularis)
- 840.6 (sprain and strain: supraspinatus)
RTC Tear Etiology / Epidemiology / Natural History
- Important factors=age, expected activity level, presence of retraction, presence of RTC muscle atrophy and fatty replacement.
- Usually >40y/o, cuff weakness, atrophy, tenderness, painful arc of motion, night pain, impingement sign, upper arm pain, painful crepitation
- Etiology: unknown, likley multifactorial includes intrinsic degeneration of tendon, poor potential for healing, vascular insufficiency, repetitive trauma, and extrinsic mechanical pressure from the surrounding coracoacromial arch. There likely is an inherited predisposition to RTC disease (Tashjian RZ, JBJS 2009;91A:1136).
- The incidence of full thickness RTC tears increases with increasing age. In cadavers under 60yrs of age the incidence of RTC tears is 6% as opposed to 30% in those over 60yrs of age. (Lehman C, Bull Hosp Jt Dis. 1995;54:30)
- Prevalence in asymptomatic patients: 0% for age 40-49yrs old; 10% for 50-59; 20% for 60-69; 40.7% for >70yrs/old. (Kim HM, JBJS 2009;91A:289).
- Asymptomatic tears are common. 13% of people aged 50-59 have asymptomatic tears. 51% of people over age 80 have asymptomatic tears. (Tempelhof S, JSES 1999:8:296)
- 25% of individuals aged in their 60s and 50% of persons aged in their 80s have full-thickness degenerative RCTs. (Tashjian R.Z. Clin Sports Med. 2012; 31: 589-604.)
- Asymptomatic tears often eventually become symptomatic.(Yamaguchi K, JSES 2001;10:199)
- Unrepaired RTC tears may progress and become irreparable. (Yamaguchi K, JSES 2001;10:199). Factors associated with progression = age >60, full-thickness tear, and fatty infliltration of the RTC muscles (Maman E, JBJS 2009;91A:1989).
- Ultrasound in patients with unilateral shoulder pain: no RTC tear average age = 48.7. unilateral tear = 58.7. Bilateral tear = 67.8. After age 60, 50% of patients have bilateral RTC tears. 35.5% of patients with symptomatic fullthickness RTC tears have tears in the asymptomatic side. (Yamaguchi K, JBJS 2006;88A:1699).
- Massive RTC may lead to Rotator Cuff Arthropathy.
- Small acute tears are easier to repair and have lower recurrence rates than large/massive tears. Long-standing tears may progress to muscle atrophy and fatty degeneration that compromises functional outcome after repair.
- Rotator cuff tears are progressive and enlarge with time and become more painful. (Keener JD, J Bone Joint Surg Am, 2015 Jan 21;97(2):89-98)
RTC Tear Anatomy
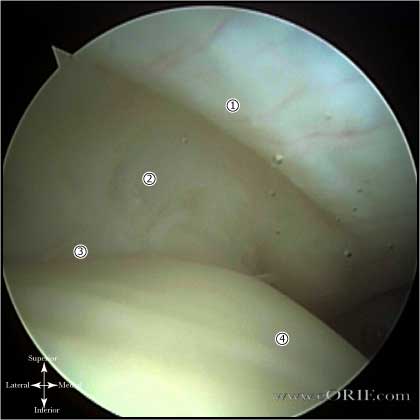
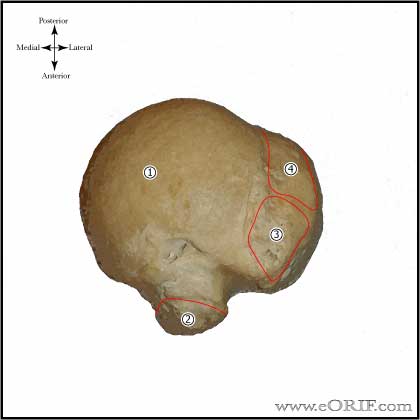
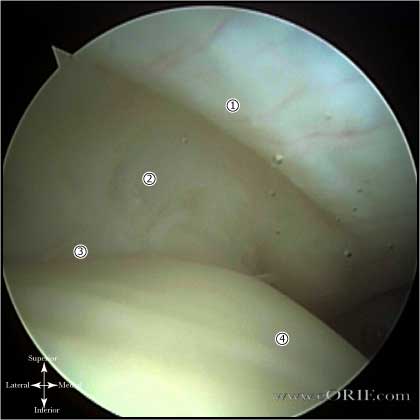
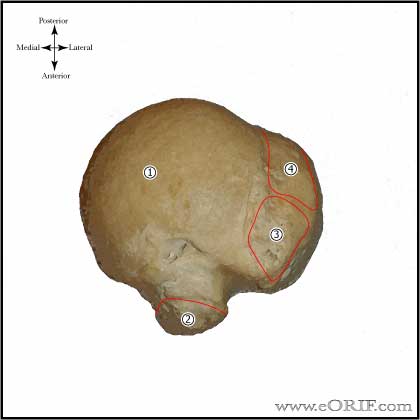
- Rotator Cable-rotator crescent complex: an arching, cable-like thickening surrounding a thinner crescent of tissue that inserts into the greater tuberosity of the humerus seen when the RTC is viewed intra-articularly. The rotator cable is 2.59 times the thickness of the rotator crescent that it surrounds and functions to stress-shield the rotator crescent. (Burkhart SS, Arthroscopy 1993; 9: 611-616)
- Halder AM, JBJS 2002;84A:780)
- Scapular spine: resembles the keel of a boat when viewed arthroscopically after excision of its surrounding subacromial fibroadipose tissue, and serves as a marker between the supraspinatus and infraspinatus
- suprascapular-nerve: At risk during the posterior interval slide. Curves tightly around the base of the scapular spine at its junction with the posterior glenoid neck, enveloped within a fat pad. The average distance from the origin of the long tendon of the biceps to the motor branches of the supraspinatus is 2 cm. The average distance from the posterior rim of the glenoid to the motor branches of the infraspinatus muscle is 2cm. (Warner JJP,JBJS 1992; 74Am: 36-45)
- Subscapularis: area= 2.41 cm2 ; Sup/Inf= 2.43 cm; M/L=1.79 cm (Dugas JR, JSES 2002;11:498).
- Supraspinatus: area=1.55 cm2 M/L=1.27: A/P=1.63 cm (Dugas JR, JSES 2002;11:498).
- Infraspinatus: area= 1.76; M/L=1.34 cm; A/P= 1.64 (Dugas JR, JSES 2002;11:498).
- Teres minor: area= 2.22 cm2; M/L=1.14 cm; A/P=2.07 (Dugas JR, JSES 2002;11:498).
- Mean total area of insertion of the rotator cuff tendons onto the greater tuberosity = 5.53 cm2. (Dugas JR, JSES 2002;11:498).
- See also Shoulder anatomy.
RTC Tear Clinical Evaluation
- Symptomatic tears have night pain, pain with overhead activity, and functional loss with daily activity. Pain is typically in the anterolateral aspect of the shoulder and often radiates toward the deltoid insertion. (Pain radiating below the elbow indicates Cervical Radiculopathy). May have clicking of popping with shoulder motion.
- Atrophy of suprspinatus and infraspinatus fossa
- A discrepancy between active and passive motion is highly suggestive of full-thickness disruption of the rotator cuff.
- Classic clinical sign of a full-thickness cuff tear is weakness with external rotation even in isolated supraspinatus tears. This is tested with the arm at the side and the elbow flexed to 90 degrees.
- Abduction weakness is associated with full-thickness RTC tears in asymptomatic shoulders (KIm MH, JBJS 2009;91A:289).
- Subscapularis is tested with lift-off test and abdominal compresison test.
- Evaluate for scapular winging. Impingement (Neer & Hawkins tests), biceps tendonitis (Speed & YergusonsTests)
RTC Tear Xray / Diagnositc Tests
- AP, scapular lateral and axillary views. . Evaluate for acromial spur, greater tuberosity sclerosis/cysts, loss of acromiohumeral interval.
- Acromiohumeral Interval: average = 10.5mm. <7mm=full-thickness RTC tear. Measure on Grashey view. (Cotty P, J Radiol 1988;16:633).
- Greater tuberosity sclerosis, osteophytes, subchondral sclerosis and osteolysis are associated with RTC tears. (Pearsall AW, JSES 2003;12:122).
- Anteroposterior (AP) view of the shoulder in external rotation, often reveals cystic changes, sclerosis, or bone reaction in the area of the greater tuberosity. In addition, a subacromial traction spur may be identified and associated AC joint pathology may be present, as reflected by cystic changes, joint narrowing, or osteophyte formation
- AP view, with a 30-degree caudal tilt, will more specifically show the anterior acromial spur; outlines the amount of acromion that projects anterior to the anterior edge of the AC joint
- Lateral extension of the acromion is associated with RTC tears. An Acromion Index (distance from the glenoid plane to the lateral border of the acromion divided by the distance from the glenoid plane to the lateral aspect of the humeral head on true A/P xray with arm in neutral rotation) of 0.73 ± 0.06 is associated with full-thickness tears: 0.64 ± 0.06is normal. (Nyffeler RW, JBJS 2006;88A:800)
- Supraspinatus "outlet" view lateral radiographic view of the scapula and acromion, with a 20-degree caudal tilt. Intended to identify any bone projecting downward into the supraspinatus outlet.
- Subacromial Morphology: Type 1= flat, Type 2 = curved, Type 3 = hooked. Acromial morphology has a noted assoicated with RTC tears (Pearsall AW, JSES 2003;12:122).
- Arthrography is the gold standard, is easily interpretable, and can clearly identify the presence or absence of a full-thickness tear. Disadvantages invasive, limited to identification of full-thickness tears only, rarely gives information about quality of the tendon or the precise location of the tendons that are torn.
- Ultrasonography: difficult to identifying small tears, partial tears, and even degenerative and scarred tissue may look similar. Operator dependent.
- MRI =highest quality image of the shoulder, precise information about the extent and location of the tendon tear, and it may give information about associated biceps instability and associated muscle atrophy or fatty infiltration. Disadvantages: patient claustrophobia, cost. Normal RTC tendon are uniformly dark on all pulse sequences. Increased signal on T1 images may be anything from artifact to complete tear. T1 abnormalities should be confirmed on T2 images. Tendinosis = intermediate signal on T1 and T2 images. Partial thickness tear = increased signal on T1 that increases to fluid signal intensity on T2 images but extends only partially through the RTC tendon. Full thickness tear = fluid (high) signal intensity completely traversing the tendon on T2 images, absence of the tendon, and retraction of the musculotendinous junction.
- In asymptomatic pts, frequency of positive MRI findings increases with patient age. In all subjects, partial and/or complete tears = 34%. In patients over 60 yrs old = 54%. (Sher JS, JBJS 1995; 77A:10)
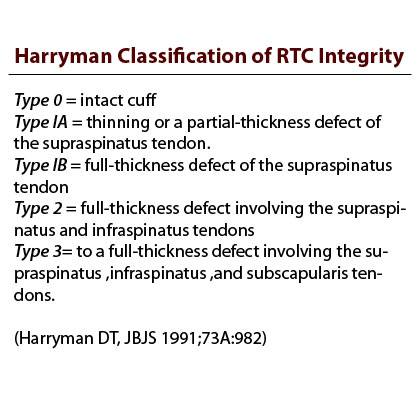
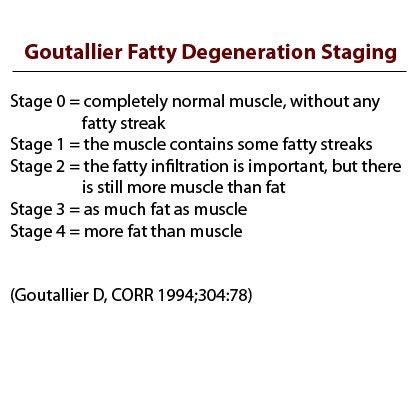
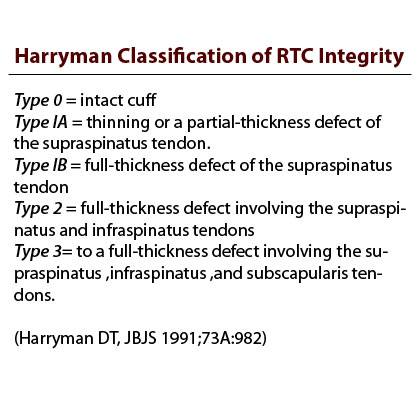
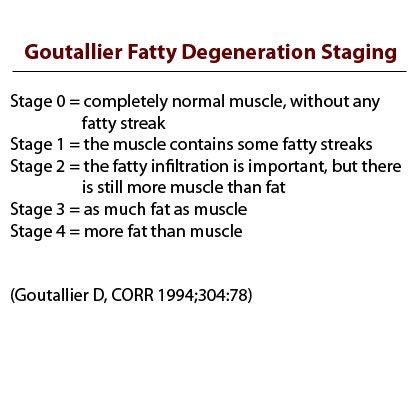
- Goutallier Classification of Muscle Atrophy (Goutallier D, CORR 1994;304:78).
-Stage 0=completely normal muscle.
-Stage 1=muscle contains some fatty streaks.
-Stage 2=fatty infiltration is important, but there is still more muscle than fat.
-Stage 3=there is as much fat as muscle.
-Stage 4=more fat than muscle is present.
-Degeneration is grade at the tip of the coracoid process and at the inferior margin of the glenoid and the values are averaged to determine the stage.
- Classification of arthritis in chronic rotator cuff tears (Hamada K, CORR 1990;254:92).
Stage 1: Acromiohumeral interval greater than 6 mm.
Stage 2: Acromiohumeral interval less than 7 mm.
Stage 3: Acromiohumeral interval less than 7 mm with acetabulization of acromion.
Stage 4a: Acromiohumeral interval less than 7 mm with glenohumeral arthritis without acetabulization.
Stage 4b: Acromiohumeral interval less than 7 mm with acetabulization and glenohumeral arthritis.
Stage 5: Acromiohumeral interval less than 7 mm with osteonecrosis of humeral head.
RTC Tear Classification / Treatment
- Asymptomatic rotator cuff tears are higly prevalent in the elderly. No treatment is required for asymptomatic tears. There is no evidence that surgery prevents long-term deterioration of a rotator cuff tear. AAOS Orthoguidelines.
- Cresent shaped: Minimal retraction, excellent mobility. Generally repaired directly to bone. See Rotator Cuff Repair.
- U-shaped: similar to cresent tears but with retraction to the glenoid rim. Even after releases the apex of the tear is difficult to mobilize. Generally repaired with margin convergence followed by repair of remaining free margin to bone. See Rotator Cuff Repair.
- L-shaped: similar to U-shaped tears, except one leaf is more mobile than the other. Generally repaired by side-to-side suturing / margin convergence followed by repair of remaining free margin down to bone. See Rotator Cuff Repair.
- Massive/contracted: no mobility from medial to lateral or anterior to posterior. Require mobilization / interval slide techniques for repair. See Rotator Cuff Repair.
- Subscapularis tears
- Partial thickness: May be managed non-operatively with PT. Shoulder arthroscopy is indicated for partial thickness tears that fail non-operative management. Consider transtendon repair of partial thickness tears that fail nonoperative managment. Tears <50% of the RTC thickness may be debrided. >50%(>6mm) can be expanded to full thickness tears and repaired. Repairs can be done via transtendon technique or completed to full-thickness tears and repaired. (Matava MJ, AJSM 2005;33:1405), (Fukuda H, JBJS 2003;85Br:3) (Kamath G, JBJS 2009;91A:1055). Untreated atraumatic partial-thickness tears have a tendency to progress to full-thickness defects. See Rotator Cuff Repair. (Yamanaka K, CORR 1994;304:68).
- AAOS Handout.
RTC Non-Operative Treatment
- Consider for older patients with chronic tears, poor tendon quality, and the presence of retraction, muscle atrophy and fatty infiltration on MRI
- NSAIDS, activity modification, ice, heat, iontophoresis, massage, TENS, PEMF, phonophoresis (ultrasound).
- Rockwood orthotherapy (home based theraband strengthening/pulley ROM) (Williams GR, JBJS 2004;86A:2764) or formal physical therapy
RTC Tear Associated Injuries / Differential Diagnosis
RTC Tear Complications
- Recurrent tear, Hardware failure / Anchor pull-out, Acromion fx, Infections, Stiffness, CRPS, Nerve injury: Axillary nerve, Brachial plexus, Fluid Extravasation:, Chondrolysis, Hematoma, Chondral Injury / arthritis, Deltoid dehiscence (open repair), Anterior-superior instability / migration.
- Recurrent tear: 5% to 15% of surgically repaired tendons will re-rupture. If adequate decompression has been done, the symptoms usually do not require further surgery
- Hardware failure / Anchor pull-out
- Acromion fx
- Infections: most common organism = Propionibacterium acnes; may require at least 7 days to culture. (Athwal GS, JSES 2007;16:306).
- Stiffness
- CRPS
- Nerve injury: Axillary nerve, Brachial plexus
- Fluid Extravasation:
- Chondrolysis: though to be related to heat from electo cautery or radiofrequency probes used during capsular release or capsular shrinkage.
- Hematoma
- Chondral Injury / arthritis
- Instrument failure
- Deltoid dehiscence (open repair)
- Anterior-superior instability / migration:
RTC Repair Follow-up care
- Abduction sling for 6 weeks with the arm in slight abduction (20°-45°, promotes better blood flow to the supraspinatus, minimize tension on the repair), may take off to eat, shower, and to use arm for desk work.
- Cryotherapy deceases pain, improves sleep and decreases need for pain medication. (Speer KP, JSES 1996;5:62).
- Must have sling on when up walking, or when sleeping
- No smoking for 8 weeks prior to surgery and 8 weeks after surgery. (Galatz LM, JBJS 2006;88A:2027).
- No NSAIDs for 6 weeks after surgery (Cohen DB, AJSM 2006;34:362).
- May drive after one week and not taking narcotic pain medications
- Start physical therapy 2-3 days post-op. Physical therapy proceeds through 4 phases. (Millett PJ, JAAOS 2006;14:599-609).
Phase 1: Passive Range of Motion (0 to 6 weeks).
Phase 2: Active Range of Motion (6 to 12 weeks).
Phase 3: Strengthening (10 to 16 weeks).
Phase 4: Advanced Strengthening (16 to 22 weeks)
- At 6-weeks discontinue sling, and begin overhead stretching.
- 12 weeks begin theraband strengthening
- Can not try to comb hair with operated arm until six weeks post-op
- Small/medium tear may play golf at 6 months
- Large/massive tear may play golf at 1 year
- Small/medium tear lift weights at 6 months
- Large/massive tears lift weights at 1 year
- Muscle atrophy and fatty inflitration is not reversable. (Fuchs JBJS 2006; Yamaguchi JBJS 2004)
- Rotator Cuff Repair Rehab Protocol
- Outcome measures: ASES score, pain scales.
- Patients referred to a specialist immediately following the diagnosis of a rotator cuff tear costs averaged $25,870.64 and returned to work an average of 7 months postoperatively. Patients managed via a “gatekeeper” system averaged $100,280.10 and return to work of 18 months. (Savoie FH, Arthroscopy 1995:11:672)
RTC Tear Review References
- Williams GR, Rockwood CA Jr, Bigliani LU, Iannotti JP, Stanwood W, Rotator Cuff Tears: Why do we repair them? JBJS 2004:86A:2764)
- Burkhart, S. S. JAAOS 2006;14:333-346.
- McConville OR, JAAOS 1999;7:32
- Burkhart SS, The Cowboy's Companion: A Trail Guide for the Arthroscopic Shoulder Surgeon, 2012
- Burkhart SS, Burkhart's View of the Shoulder: A Cowboy's Guide to Advanced Shoulder Arthroscopy, 2006
- AANA Advanced Arthroscopy: The Shoulder: Expert Consult: Online, Print and DVD, 1e, 2010
- OKO Rotator Cuff
|