|







|
synonyms: proximal humerus fracture,
Proximal Humerus Fx ICD-10
A- initial encounter for closed fracture
B- initial encounter for open fracture
D- subsequent encounter for fracture with routine healing
G- subsequent encounter for fracture with delayed healing
K- subsequent encounter for fracture with nonunion
P- subsequent encounter for fracture with malunion
S- sequela
Proximal Humerus Fx ICD-9
- 812.0_(closed); 812.1_(open)
- 812._0(fracture of humerus, upper end, unspecified)
- 812._1(fracture of humerus, upper end, surgical neck)
- 812._2(fracture of humerus, upper end, anatomic neck)
- 812._3(fracture of humerus, upper end, greater tuberosity)
- 812._9(fracture of humerus, upper end, other; head, upper epiphysis)
Proximal Humerus Fx Etiology / Epidemiology / Natural History
- Majority occur in the elderly (fracture of senescence), are minimally displaced and stable.
- Third most common fracture in patients >60 years of age.
- In patients >60years the majority occur from a simple fall. In young patients they generally involve high-energy trauma.
- 15-20% have significant displacement, angulation, malrotation or GT involvement.
- Female:male = 2:1. 60 year old woman has on 8% risk of lifetime proximal humerus fracture (Lauritzen JB, Osteoporos Int 1993;3:127).
- Represent 5% of all fractures. 3rd most common fracture type.
- Risk factors: osteoporosis, advance age. (Kannus P, Acta Orthop Scand 2000:71:465).
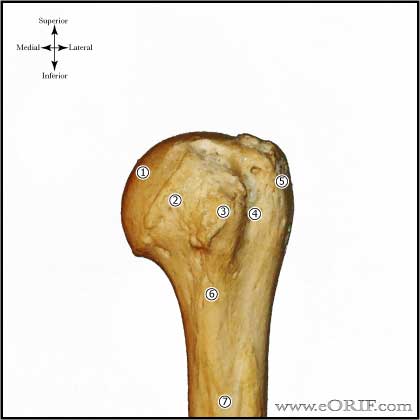
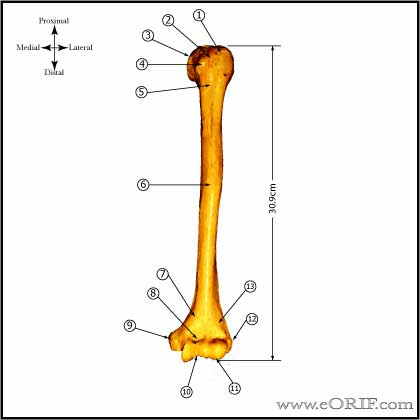
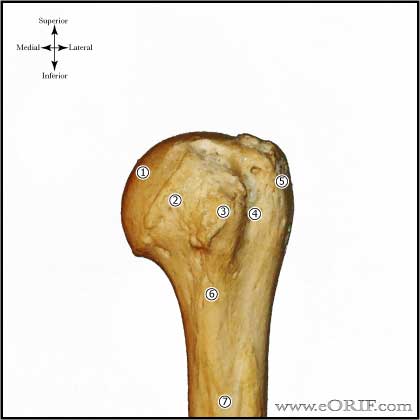
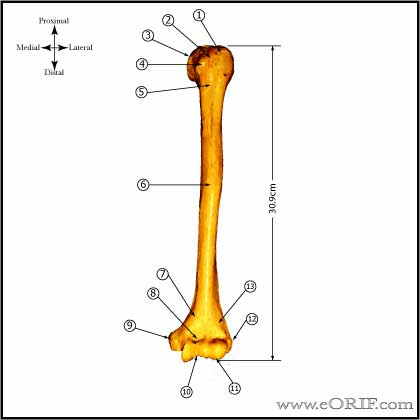
Proximal Humerus Fx Anatomy
- Anatomic Landmarks
-Mean distance between the pectoralis major tendon and the top of the humeral articular surface is 5.6cm (Murachaovsky J, JSES 2006;15:675).
-Normal distance from the greater tuberosity to the superior protion of the articular surface of the humeral head = 7-8mm (Iannotti JP, JBJS 1992;74A:491), (Takase K, JSES 2002;11:557).
-The neck-shaft inclination angle averages 145 degrees. The humeral head is retroveted an average of 30 degrees.
- Greater tuberosity = insertion of supraspinatus, infraspinatus, and teres minor tendons
- Lesser tuberosity = insertion of subscapularis tendon.
- Displaced greater tuberosity fx is pathognomonic of a longitudinal tear in the rotator cuff at the rotator interval between the supraspinatus and subscapularis tendons.
- Primary blood supply to humeral head is the ascending (arcuate) branch of anterior humeral circumflex artery which runs in the bicipital groove.(Jaberg, JBJS 74A:508;1992) Less significant supplies include the posterior humeral circumflex artery and small vessels enteriing through the rotator cuff insertions. (Brooks CH, JBJS 1993;75Br:132).
- Humeral head vascularity after fracture can be estimated by the amount of metaphyseal head extension, <8mm is associated with ischemia; Medial hinge disruption >2mm is associated with ischemia. If both indicate ischmia the positive predictive value of ischemia for an anatomic neck fx is 97%. (Hertel R, JSES 2004;13:427).
- Most common site of injury to the axillary artery is in the third part(named in relation to the pec minor) of the artery at the origin of the anterior and posterior humeral circumflex arteries.
- Deforming forces: Pectoralis major pulls the shaft medially, anteriorly and internally rotates. Supraspinatus abducts the head fragment in two part fractures. If greater tuberosity is fractured it is pulled superiorly and posteriorly by the supraspinatus and infraspinatus. Lesser tuberosity fractures are pulled medially.
- see also Shoulder Anatomy.
Proximal Humerus Fx Clinical Evaluation
- Generally complain of shoulder pain after a fall
- Swelling and ecchymosis in shoulder which can expend into chest wall and down arm.
- Document NV exam, especially axillary nerve.
- Assess for head injury, LOC, cardiac/neurologic reasons for fall.
Proximal Humerus Fx Xray / Diagnostic Tests
- AP, scapular lateral and axillary views. Ensure humeral head is not dislocated.
- AP in external rotation best demonstrates greater tuberosity fractures. AP in internal rotation best demonstrates lesser tuberosity fractures.
- Predictors of humeral head ischemia are length of the metaphyseal head extension (accuracy, 0.84 for calcar segments <8 mm), and the integrity of the medial hinge (accuracy, 0.79 for disrupted hinge). https://doi.org/10.1016/j.jse.2004.01.034
- CT may be useful in determining fracture type (head splitting) and displacement, especially in greater tuberosity fractures. Helpful for pre-op planning.
- MRI generally not useful.
- Consider EMG/NCV if neurologic injury is suspected, occurs in 67% of proximal humerus fractures. (Visser CP, JSES 2001;10:421).
- Angiogram: consider for diminished radial/brachial pulse, expanding hematoma, changing neurologic status.
Proximal Humerus Fx Classification / Treatment
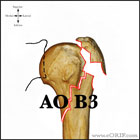
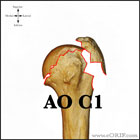
- Neer classification based on parts(shaft, head, GT, LT); displacement = >10mm or >45 degree angulation. (Neer CS II, JBJS 1970;52A:1077). Poor interobserver reliability (Sidor ML, JBJS 1993;75A:1745) CT improves interobserver reliablity(Edelsen G, JBJS 2004;86Br:413).
- Minimally displaced = sling, PT within 2 wks. Functional outcome, ROM and pain are significantly better when PT is started within first two weeks. (Koval JBJS 1997;79A:203). (Hodgson SA, JSES 2007;16:143).
- Proximal Humerus Surgical Indications: fx 1cm displaced or have >45 degrees angulation or >10mm tuberosity displacement, open fx, unable to reduce by closed means,
- Greater tuberosity 2-part fracture
- Surgical neck 2-part fracture
- Lesser tuberosity 2-part fracture
- Valgus impacted 4-part fx with good bone: ORIF. Non-op outcomes = 80% adjusted Constant score (Court-Brown CM, JBJS 2002;84Br:504)
- 4-Part Fracture: insufficient evidence is available to determine best treatment option (Bhandari M, JOT 2004;18:126). Increased pain with non-op treatment, equivalent ROM. Poor results demonstrated with non-op treatment (
- RSA within 4 weeks of injury results in improved external rotation and decreased complications and scapular notching compared to RSA done >4 weeks from injury. (Seidl A, ASES Specialty Day 2017)
- Hemiarthroplasty outcomes are dependent on anatomic healing of the tuberosities around the implant. Greater tuberosity displacement or reabsorption leads to significant loss of active motion. Reverse TSA outcomes are less dependent on , anatomic tuberosity healing.
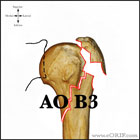
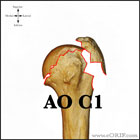
- AO Classification
- Pediatric Proximal Humerus fracture.
- Proximal Humerus Fracture CRPP 23615
- Proximal Humerus Fracture Hemiarthroplasty 23616
- Proximal Humerus Fracture ORIF 23615
- increased AVN. Beach chair position, deltopectoral approach, mobilize cephalic vein medially, release all or part of deltoid insertion, incise clavipectoral fascia, visualize/repair fracture. Techniques include screws with tension bands, locked plates, plates
- Synthes proximal humeral locking plate-plate should be 8mm distal to RTC insertion, higher placement=subacromial impingement, Remember to remove insertion guide.
- Three-part fx =open reduction and that for four-part fractures was prosthetic replacement. Using these indications, the typical result was satisfactory but imperfect and many months were required for maximum recovery. In Neer’s study, closed treatment appeared inadequate for active patients. Open treatment (N=38) using suture fixation of the tuberosities and cuff repair yielded satisfactory results or excellent results in 86%.
- Proximal Humerus Nonunion: (Antuna SA, JSES 2002;11:114), (Boileau P, JSES 2001;10:299).
Proximal Humerus Fx Associated Injuries / Differential Diagnosis
Proximal Humerus Fx ORIF/CRPP Complications
- Hardware failure
- Stiffness
- Pain
- Avascular necrosis of humeral head: high risk with anatomic neck fracture, short medial metaphyseal extension, disruption of the medial periosteal hinge. (Hertel R, JSES 2004;13:427).
- Nonunion: tuberosity nonunion is most common
- Malunion: tuberosity malunion >2cm below the humeral head is associated with poor outcomes (Mighell MA, JSES 2003;12:569).
Proximal Humerus Fx Hemiarthroplasty Complications
- (Plausinis D, JBJS 2005:87A;204).
- Infection
- Nerve palsy: axillary, radial, median, musculocutaneous, brachial plexus
- Fracture: intraoperative / postoperative periprosthetic
- Instability
- rotator cuff tear, proximal migration
- loosening
- Heterotopic ossification
- Glenoid DJD
- Stiffness
- Complex Regional Pain Syndrome
Proximal Humerus Fx Follow-up Care
- Post-op/Initial non-op: Sling, gentle pendelum ROM
- 2-3 weeks: gentle passive ROM. No rotation motions. Early PT improves outcomes in minimally displaced fractures (Koval KJ, JBJS 1997;79A:203).
- 5-6 weeks: begin IR/ER passive ROM exercises. Progress to active and active-assisted ROM.
- Recovery of motion is greatest difficulty, especially after surgery and in 4-part fractures were motion must be restricted until union of tuberosities is evident.
- Proximal Humerus Fracture Rehab Protocol.
- Shoulder Outcome Measures.
Proximal Humerus Fx Review References
- Neer CS II: Displaced proximal humeral fractures: II. Treatment of three-part and four-part displacement. J Bone Joint Surg Am 1970;52:1090-1103.
- Rockwood and Green's Fractures in Adults 6th ed, 2006
- Nho SJ, JAAOS 2007;15:12
- Cadet ER, Ahmad CS, Hemiarthroplasty for three- and four-part proximal humerus fractures. J Am Acad Orthop Surg 2012;201(1):17-27. PMID: 22207515.
- Greiwe RM, Vargas-Ariza R, Bigliani LU, Levine WN, Ahmad CS. Hemiarthroplasty for head-split fractures of the proximal humerus. Orthopedics 2013;36(7):e905-911. PMID: 23823048.
- Solberg BD, Moon CN, Franco DP, Paiement GD. Surgical treatment of three- and four-part proximal humerus fractures. J Bone Joint Surg Am 2009;91(7):1689-1697. PMID: 19571092.
- Hettrich CM, Neviaser A, Beamer BS, Paul O, Helfet DL, Lorich DG. Locked plating of the proximal humerus using an endosteal implant. J Orthop Trauma 2012;26(4):212-215. PMID: 22337487.
- Boileau P, Krishnan SG, Tinsi L, Walch G, Coste JS, Mole D. Tuberosity malposition and migration: reasons for poor outcomes after hemiarthoplasty for displaced fractures of the proximal humerus. J Shoulder Elbow Surg 2002;11(5):401-412. PMID: 12378157.
- Krishnan SG, Reineck JR, Bennion PD, Feher L, Burkhead WZ Jr. Shoulder arthroplasty for fracture: does a fracture-specific stem make a difference? Clin Orthop Relat Res 2011;469(12):3317-3323. PMID: 21598120.
- Bufquin T, Hersan A, Hubert L, Massin P. Reverse shoulder arthroplasty for the treatment of three- and four-part fractures of the proximal humerus in the elderly: a prospective review of 43 cases with a short-term follow-up. J Bone Joint Surg Br 2007;89(4):516-520. PubMed PMID: 17463122.
- Robinson CM, Page RS. Severely impacted valgus proximal humeral fractures. J Bone Joint Surg Am 20004;86(Supp 1):143-155. PMID: 15466755.
- Namdari S, Horneff JG, Baldwin K. Comparison of hemiarthroplasty and reverse arthroplasty for treatment of proximal humeral fractures: a systematic review. J Bone Joint Surg Am. 2013 Sep 18;95(18):1701-8. doi: 10.2106/JBJS.L.01115.
- Moineau G, McClelland WB Jr, Trojani C, Rumian A, Walch G, Boileau P. Prognostic factors and limitations of anatomic shoulder arthroplasty for the treatment of posttraumatic cephalic collapse or necrosis (type-1 proximal humeral fracture sequelae). J Bone Joint Surg Am. 2012 Dec 5;94(23):2186-94. doi: 10.2106/JBJS.J.00412.
- Jarrett CD, Brown BT, Schmidt CC. Reverse shoulder arthroplasty. Orthop Clin North Am. 2013 Jul;44(3):389-408, x. doi: 10.1016/j.ocl.2013.03.010. Epub 2013 Apr 29.
- Anakwenze OA, Zoller S, Ahmad CS, Levine WN. Reverse shoulder arthroplasty for acute proximal humerus fractures: a systematic review. J Shoulder Elbow Surg. 2014 Apr;23(4):e73-80. doi: 10.1016/j.jse.2013.09.012. Epub 2014 Jan 7
- Südkamp N, Bayer J, Hepp P, Voigt C, Oestern H, Kääb M, Luo C, Plecko M, Wendt K, Köstler W, Konrad G. Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate. Results of a prospective, multicenter, observational study. J Bone Joint Surg Am. 2009 Jun;91(6):1320-8. doi: 10.2106/JBJS.H.00006.
- Hertel R, Hempfing A, Stiehler M, Leunig M. Predictors of humeral head ischemia after intracapsular fracture of the proximal humerus. J Shoulder Elbow Surg. 2004 Jul-Aug;13(4):427-33.
- Hartmann A, Resch H, OKU-Shoulder and Elbow 3rd edition, 2008
|