|
|
synonyms:
Pediatric Brachial Plexus Palsy ICD-9
Pediatric Brachial Plexus Palsy Etiology / Epidemiology / Natural History
- 0.1%-0.4% of live births
- most show signs of recovery in first 2 months of life, and usually will subsequently have normal function.
- recovery monitored by elbow flexion, shoulder abduction, and extension of wrist, fingers and thumb.
- If minimal recovery after 3-6months permanent impairment is likely and surgery invention may be beneficial.
- total plexus lesion, partial plexus lesion with C5-C7, or Horner’s syndrome =worse prognosis
Brachial Plexus Risk factors
- large babies
- multiparous pregnancy
- shoulder dystocia
- forceps delivery
- prolonged labor
- breech
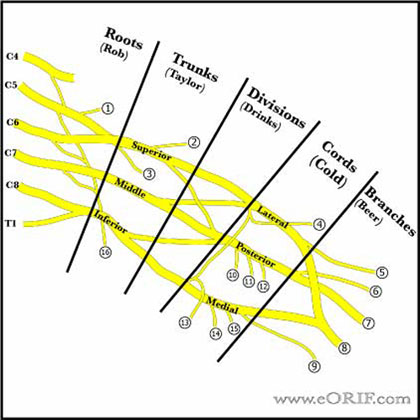
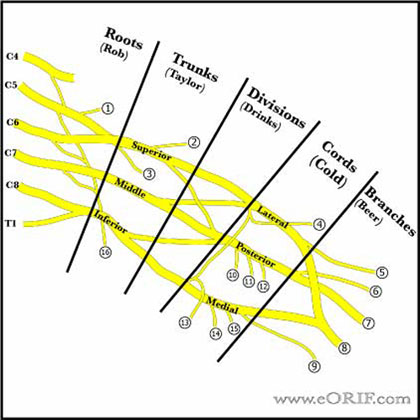
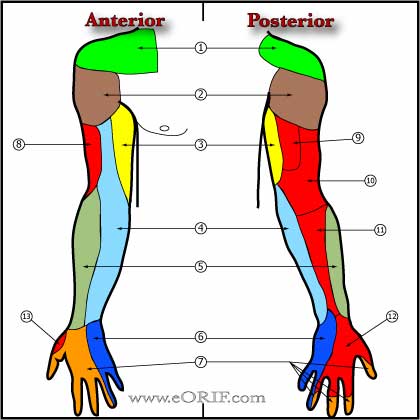
Pediatric Brachial Plexus Palsy Anatomy
- C5-T1(77%), C4-T1(22%), C5-T2(1%)
- ganglion is adjacent to spinal cord and contains sensory cell body
- Preganlionic lesions are avulsions of the cord and will not spontaneously recover
- Upper limb bud appears during the fourth week of gestation and develops from the fifth to the eighth week of gestation.
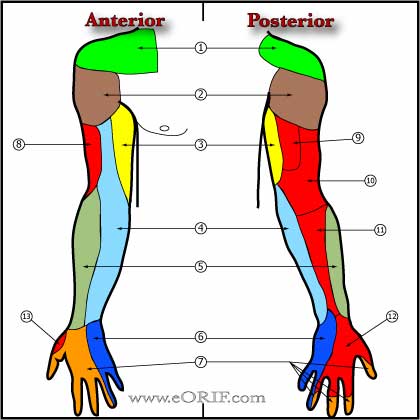
Pediatric Brachial Plexus Palsy Clinical Evaluation
- Horner’s syndrome(sympathetic chain), elevated hemidiaphragm(phrenic nerve), rhomdoid(subscapular n), supraspinatus(suprascapular n), latismus dorsi(thoracodorsal) or winged scapula(long thoracic n) concerning for preganglionic injury. Preganglionic injury=poor prognosis for recovery.
- positive histamine response implies that the reflex arc between the afferent nerves, effernent nerves, and an intervening cell body, or ganglion is intact and indicates the injury is proximal to the ganglion ie preganglionic
Pediatric Brachial Plexus Palsy Xray / Diagnositc Tests
- upper limb, clavicle C-spine
- MRI of the shoulder is indicated for patients whos passive ROM fails to improve with Physical Therapy to evaluate for increased glenoid retroversion and/or posterior shoulder subluxation.
Pediatric Brachial Plexus Palsy Classification / Treatment
- Erb's Palsy -C5,C6(upper trunck)-most common-generally postganglionic-deltoid, supraspinatus, infraspinatus, teres minor, biceps, brachialis, supinator, brachioradialis, +/-wrist & hand dorsiflexors. Best prognosis
- Klumpke's Palsy -C8,T1(lower trunk)-rare-generally preganglionic-wrist flexors, intrinsics, Horners. Prognosis poor. Leads to elbow flexion and forearm suppination contracture.
- x-C5-T1-upper limb almost completely flaccid
- Initial Treatment: passive ROM of all joints especially GH joint with scapulothoracic joint stabilized, may need PT. MRI of the shoulder is indicated for patients whos passive ROM fails to improve with Physical Therapy to evaluate for increased glenoid retroversion and/or posterior shoulder subluxation. Consider botulinum toxin-A injection (1iu/kg) into the pec major, teres major and subscapularis under general anesthesia with shoulder stretching and shoulder spica placement (arm abduceted, elbow flexed 90°) for 4 weeks for patients with high potential for shoulder dysplasia.
- Brachial plexus exploration with sural nerve graft reconstruction is indicated for infants with totoal plexopathy associated with Horner's Syndrome at 3 months and between 3-9months for patients without return of biceps function.
- long standing pts develop IR contracture and ER weakness. Upper trunk injuries with Intact adductors and IR with weak abductiors and ER leads to progressive GH deformity close to 70% with significant ER limitations develop glenoid dysplasia. Suggest early subscapularis release if unresponsive to PT vs anterior pec major release with latismus and teres major transfers. Humeral derotational osteotomy is indicated for unreconstructable shoulders. (Waters PM, JBJS 2005;87A:320), (Pearl ML, JBJS 2006;88A:564).
Pediatric Brachial Plexus Palsy Associated Injuries / Differential Diagnosis
- humerus fx
- prox hum fx
- clavicle fx
- acute humeral osteomyelitis
- GH septic arthritis
- consider spinal cord tumor or CP if seen later in life
Pediatric Brachial Plexus Palsy Complications
Pediatric Brachial Plexus Palsy Follow-up Care
Pediatric Brachial Plexus Palsy Review References
- Geutjens G, et al: Obstetric brachial plexus palsy associated with breech delivery: Adifferent pattern of injury. JBJS Br. 1996,78:303-306
- Waters PM: Obstetric brachial plexus injuries: Evaluation and management. JAAOS 1997; 205-214
- Clarke HM, Hand Clin 1995;11:563
|