|
|
synonyms: acute brachial neuritis, BN, brachial plexitis, brachial radiculitis, Parsonage-Turner syndrome, shoulder girdle syndrome
Parsonage-Turner Syndrome ICD-10
- G54.0: Brachial plexus disorders
Parsonage-Turner Syndrome ICD-9
- 353.0 Brachial plexus lesions: Cervical rib syndrome, costoclavicluar syndrome, scalenus anticus syndrome, thoracic outlet syndomre
Parsonage-Turner Syndrome Etiology / Epidemiology / Natural History
- Brachial neuritis.
- Rare
- Etiology unknown; may be inflammatory or immune-mediated mechanism.
- Males > females
- 25% bilateral
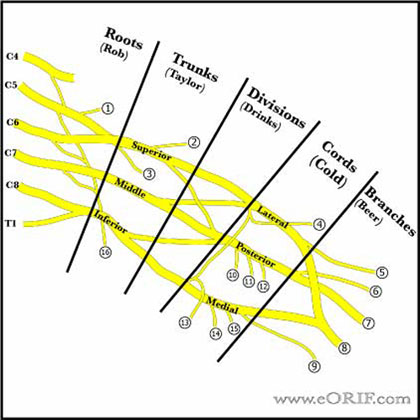
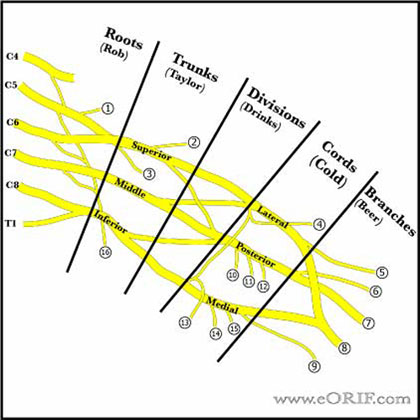
Parsonage-Turner Syndrome Anatomy
- Brachial plexus is formed from C5, C6, C7, C8, and T1 nerve roots. There may be contributions from C4, and T2. A plexus with contributions from C4 is called “prefixed.” (28% to 62%). "Postfixed" = contributions from T2 (16% to 73%). (Kerr AT, Am J Anat 1918;23:285).
- Roots and trunks are more commonly affected than the divisions, cords, or terminal branches.
- Trapezius and levator scapulae muscles are almost always intact after traumatic brachial plexus injury allowing for active arm abduction through the scapulothoracic articulation.
- If serratus anterior function is preserved, forward elevation of the arm through scapular rotation is possible.
- Preganglionic injury = spinal roots are avulsed from the spinal cord; little potential for recovery. Postganglionic = distal to the dorsal root ganglion; some potential for spontaneous recovery.
- Avulsion of the T1 root (a pre-ganglionic injury) interrupts the T1 sympathetic ganglion,c ausing Horner's syndrome (miosis (small pupil), enophthalmos (sinking of the orbit), ptosis (lid droop), and anhydrosis (dry eyes).
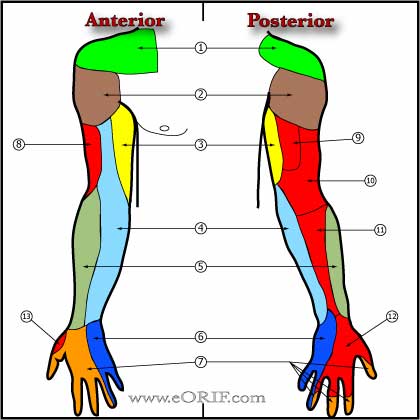
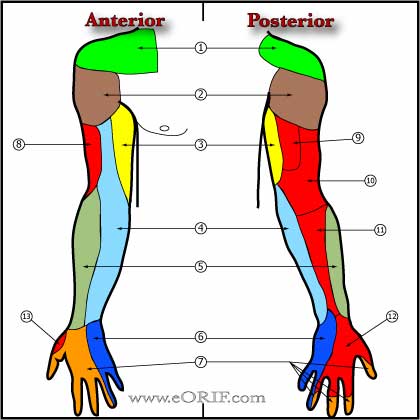
- Injury to C5,C6,C7 may result in loss of shoulder flexion, elbow fexion and extension and occasionally wrist and finger extension.
- Injury to C8 and T1 may limit hand function.
- Upper trunk = C5,C6 = rhomboids, deltoid, infraspinatus, brachioradialis.
- Middle trunk = C7 = pronator teres, extensor carpi radialis
- Lower trunk = C8 = extensor carpi ulnaris, flexor carpi ulnaris, flexor pollicis longus.
Parsonage-Turner Syndrome Clinical Evaluation
- Generally associated with a viral prodrome and significant pain.
- Acute excruciating unilateral shoulder pain, followed by flaccid paralysis of shoulder and parascapular muscles several days later.
- Varies greatly in presentation and nerve involvement. * Due to the extreme pain involved, patients usually present acutely. Typically, the affected arm is supported by the uninvolved arm and is held in adduction and internal rotation.
- May have atrophy of the affected muscles
- Pain with palpation and active and passive ROM
- Reflexes may be reduced/absent, depending on nerves involved.
- Sensory loss generally not prominent; may be detectable depending nerves involved (axillary nerve sensation).
- May cause scapular winging.
Parsonage-Turner Syndrome Xray / Diagnositc Tests
- C-spine, shoulder (anteroposterior and axillary views), and chest views indicated. generally normal
- MRI: consider to rule out other potential diagnoses.
- EMG/NCV: Consider serial EMG/NCV with repeat physical examination to document and quantify reinnervation or denervation. Fibrillations = denervation.
Parsonage-Turner Syndrome Classification / Treatment
- Observation with physical therapy focused on the maintenance of full ROM of the shoulder and other affected joints. PROM and AROM exercises. Consider heat, cold, transcutaneous electrical nerve stimulation as adjunct pain relievers.
Parsonage-Turner Syndrome Associated Injuries / Differential Diagnosis
- Axillary artery rupture / injury
- Burner Syndrome
- Thoracic Outlet Syndrome
- Paget Schroetter
- Parsonage-Turner Syndrome
- Carpal tunnel syndrome
- Brachial plexus injury
- Adhesive capsulitis
Parsonage-Turner Syndrome Complications
- Contractures
- Pain syndromes
- Loss of function
Parsonage-Turner Syndrome Follow-up Care
- Follow with serial physical exams +/- EMG/NCV to monitor for improvements and ensure PROM is maintained in affected joints.
- Consider nerve grafting or tendon transfers if no improvement has occur after 2 years of observation.
Parsonage-Turner Syndrome Review References
- Magee KR, JAMA 1960;174:1258
- Misamore GW, JBJS 1996;78A:1405
- McCarty EC, CORR 1999;368:37
|