|
|
synonyms: multidirectional instability, MDI
MDI ICD-10
MDI ICD-9
- 718.31 Recurrent shoulder dislocation
- 718.81 (other shoulder joint derangement, not elsewhere classified, instability of shoulder joint)
MDI Etiology / Epidemiology / Natural History
- Global shoulder laxity (anterior, posterior and inferior) which produces symptoms inferiorly and in at least one other direction.
- Multifactorial etiology; may include loose redundant inferior pouch, large rotator interval, aberrant muscle firing patterns, abnormal connective tissue, activity related demands, glenoid anatomy.
- May have preceeding traumatic dislocation, repetitive microtrauma with overhead acitivity, or generalzed ligamentous laxity.
- Gymnastics, volleyball, weightlifters, butterfly swimming, raquet/throwing sports may result in repetitive microtrauma and GH laxity.
- Congenital etiologies: collagen disorders; Ehlers-Danlos syndrome, Marfans Syndrome. Often have family history
- Generally younger than 35y/o.
- Male = Female
MDI Anatomy
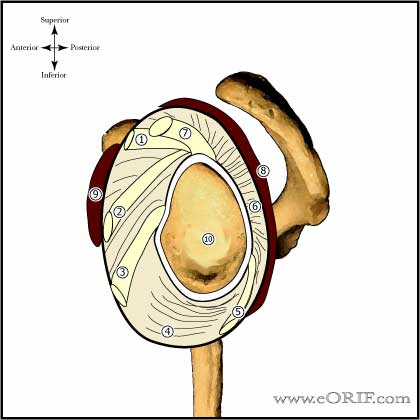
- Glenohumeral stability is dependent on static (labrum, GH capular ligmants) and dynamic (RTC, deltoid, biceps, scapular musculature) restraints.
- Inferior glenohumeral ligament (consist of anterior inferior GH ligamant, axillary pouch and posterior inferior GH ligament) is the most important for resisting anterior translation in the abducted arm.
- Hidden lesions of the posterior labrum may be present (Kim SH, Arthroscopy 2004;20:712).
- MDI patients frequently have a cleft in or absense of the rotator interval (Harryman DT, JBJS 1992;74A:53)
MDI Clinical Evaluation
- Generally young, female athletes, c/o early fatigue, weakness, dead arm symptoms, pain, instability, weakness, paresthesias (inferior instability), popping, grinding, clicking.
- Anterior instability=symptoms when in apprehension position such as cocking arm to throw (abduction, ER), reaching overhead, sleeping with arm overhead.
- Posterior instability=slips out with forward elevation/IR such as removing book from overhead shelf, blocking for football linemen.
- Interior instability=carrying heavy objects at side may also have traction paresthesias.
- Generalized ligamentous laxity=hyperextension of elbows, knees, MCP joints, hyperabduction of thumb, patellofemoral laxity
- Sulcus sign, load and shift, Push-pull test.
- Evaluate for Scapular dyskinesia.
- Assessments of generalized ligamentous laxity: ability to touch ipsilateral forearm with the thumb, place palms of hands on floor with knees locked, elbow/knee/MCP hyperextension.
- Must rule out psychological problems/ voluntary dislocators!
- Assess for history of Ehlers-Danlos or Marfan Syndrome.
MDI Xray / Diagnositc Tests
- A/P and Lateral view in the plane of the scapula, and axillary view.
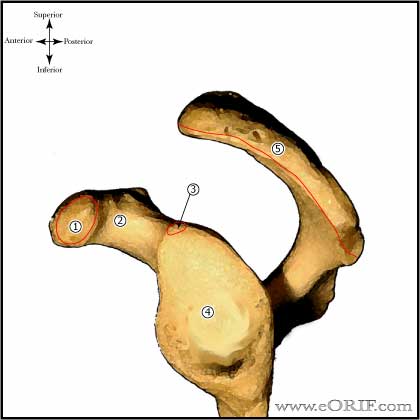
- AP views in IR & ER, Stryker notch view, apical oblique view. Evaluate for Bankart lesion and Hill-Sachs lesion. Glenoid hypoplasia/retroversion
- West Point view: Useful for evaluating the anterior glenoid rim / bony Bankart lesions.
- Hill-Sachs lesion: impression fracture of the posterosuperior aspect of the humeral head, produced by contact with the anteroinferior glenoid when dislocated. Hill-Sachs lesion is demonstrated on plain AP radiograph in internal rotation or Stryker notch view.
MDI Classification / Treatment
- Initial treatment: 6 months physical therapy: RTC co-contraction, deltoid, scapular stabilizer strengthening, improve proprioception, correct any abnormal muscle firing. >80% success rate. Nonsurgically treated young, athletic patients: 49% significant pain, 46% continued instability, 37% go on to have surgical treatment. By the modified Rowe grading scale 14% excellent results, 33% good, 53% poor results. (Misamore GW, JSES 2005;14:466).
- Consider Shoulder Pacemaker functional E-stim muscle training.
- Surgical treatment: arthroscopic capsular plication / rotator interval closure vs open anterior-inferior Capsular shift. Arthorscopic Capsular Plication: 97% good/excellent results (Kim SH, AJSM 2004;32:594). Closure of the rotator interval has not been definitively shown to enhance stability or improve outcomes for patients with MDI.
MDI Associated Injuries / Differential Diagnosis
MDI Complications
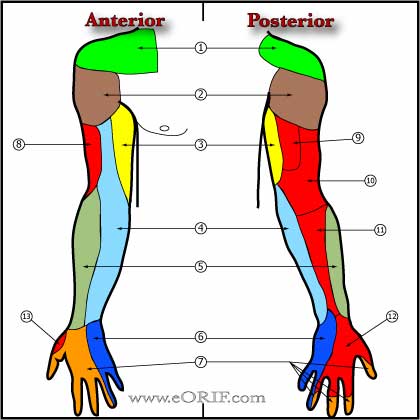
- Neurologic injury; 8.2% incidence after anterior reconstruction for recurrent GH instability. 78% recover completely. (Ho E, JSES 1999;8:266-270). Axillary nerve, Brachial plexus
- Loss of ER, with eventual GH DJD.
- Recurrent MDI
- Pain
- Hardware failure / Anchor pull-out
- Infections
- Stiffness
- CRPS
- Fluid Extravasation:
- Chondrolysis: though to be related to heat from electo cautery or radiofrequency probes used during capsular release or capsular shrinkage.
- Hematoma
- Chondral Injury / arthritis
- Instrument failure
- Weakness
MDI Arthroscopic Plication Follow-up care
- Post-op: shoulder immobilizer, remove dressing at 72 hrs, replace dressing, may shower if dry, replace dressing after each shower.
- 7-10 Days: Pendelum exercises, passive FE with overhead pulley, gentle passive ER with a stick 4-6 times daily. Limit of ER is determined at surgery. Elbow wrist hand ROM. Sling contiuously for 2-3 weeks, with activity thereafter.
- 6 Weeks: Advance to stregthening. Full active ROM.
- 3 Months: Sport specific training.
- 6 Months: Return to sport/heavy labor at 5-8months depending on regaining 90% of strength.
- 1Yr: Mid-range stability is mainly dependent on muscular balance and coordination. Lifelong rehab program is required.
- Shoulder Outcome measures
MDI Review References
|