|




|
synonyms: hip fracture, femoral neck fracture, femoral neck fx
Femoral Neck Fracture ICD-10
- S72.001A - Fracture of unspecified part of neck of right femur, initial encounter for closed fracture
- S72.002A - Fracture of unspecified part of neck of left femur, initial encounter for closed fracture
- S72.031A - Displaced midcervical fracture of right femur, initial encounter for closed fracture
- S72.032A - Displaced midcervical fracture of left femur, initial encounter for closed fracture
- S72.034A - Nondisplaced midcervical fracture of right femur, initial encounter for closed fracture
- S72.035A - Nondisplaced midcervical fracture of left femur, initial encounter for closed fracture
- S72.041A - Displaced fracture of base of neck of right femur, initial encounter for closed fracture
- S72.042A - Displaced fracture of base of neck of left femur, initial encounter for closed fracture
- S72.044A - Nondisplaced fracture of base of neck of right femur, initial encounter for closed fracture
- S72.045A - Nondisplaced fracture of base of neck of left femur, initial encounter for closed fracture
Femoral Neck Fracture ICD-9
- 820.00(closed unspecified intracapsular) 820.10(open unspecified intracapsular)
- 820.01(closed ephiphseal separation) 820.11(open ephiphseal separation)
- 820.02(closed midcervical) 820.12(open midcervical)
- 820.03(closed base of neck) 820.13(open base of neck)
- 820.09(closed other, head of femur, subcapital) 820.19 (open other)
Femoral Neck Fracture Etiology / Epidemiology / Natural History
- Intracapsular proximal femur fractures that occur distal to the articular surface of the femoral head and proximal to the intertrochanteric region.
- overall 1 yr mortality in the elderly ranges from 14-36%, highest within first 4-6 months
- There is an increased risk of mortality with delay in surgical treatment. (Bottle A, BMJ 2006;332:947).
- Preoperative risk factors associated with postoperative mortality: chronic renal failure, congestive heart failure, chronic obstructive pulmonary disease, age of older than 70 years. (Bhattacharyya T, J Bone Joint Surg Am. 2002 Apr;84-A(4):562-72)
- primarily pts >50y/o
- females>males 3.4/1
Hip Fx Risk Factors
- age >50
- caucasion female
- urban dwelling
- smoking
- excessive alcohol or caffine intake
- physical inactivity
- previous hip fx
- significant weight loss in midlife
- psychotropic medications
- senile dementia
- postmenarche
- institutionalization
- History of stroke
- Parkinson's disease: consider anterior approach and correction of hip adduction contracture by tenotomy if treating with hemiarthroplasty.
- Proton pump inhibitors (Prevacid, Nexium, Prilosec, Protonix, Aciphex)
- Histamine-2 receptor antagonists, or H2RAs, (Zantac, Tagamet).
Femoral Neck Fracture Anatomy
- Lateral epiphyseal artery, which is the terminal branch of the medial femoral circumflex artery of the profunda femoris circulation supplies the majority of the femoral head.(Trueta, JBJS 35B:442;1953).
- Blood supply to femoral neck=extracapsilar arterial ring at base of neck supplied by branches of lateral and medial femoral circumflex artery, ascending cervical branches of arterial ring on surface of the neck, arteries of the ligamentum teres.
- Fractures are usually entirely intracapsular thus bath in synovial fluid which may interfere with healing.
- Neck has essentially no periosteal layer thus healing must be endosteal
- Neck shaft angle = 130+/-7
- Femoral neck anterversion =10.4+/-6.7
- Femoral head diameter = 40-60mm
- Calcar femorale is a condensed, vertically oriented plate of bone within the proximal femur.
Femoral Neck Fracture Clinical Evaluation
- Generally non-ambulatory after fall onto the affected hip. Complain of hip or groin pain which is exacerbated by any hip ROM.
- Displaced fractures generally have obvious deformity with affected leg shortened and externally rotated.
- Complete neurovascular exam indicated.
- Pre-operative medical clearance indicated for elderly patients.
Femoral Neck Fracture Xray
- A/P pelvis and A/P & cross-table lateral of hip. Non-displaced fractures can be difficult to see on plain films. Consider 15 degree internal rotation A/P which allows visualization of the entire femoral neck.
- MRI is indicated to evaluate for occult hip fracture. MRI can be performed within 24 hrs of injury and is more accurate and cost-effective than bone scanning in diagnosing occult hip fx. Early MRI does not help predict the development of AVN.
- Bone scan is sensitive at diagnosing occult hip fracture but is not diagnostic for 48-72 hrs after injury. Consider bone scan if MRI is not available.
Femoral Neck Fracture Classification/Treatment
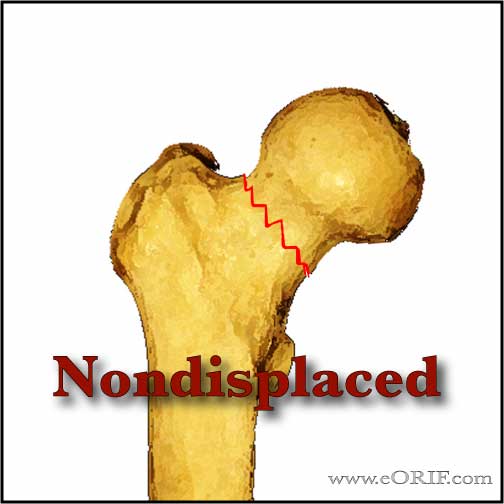
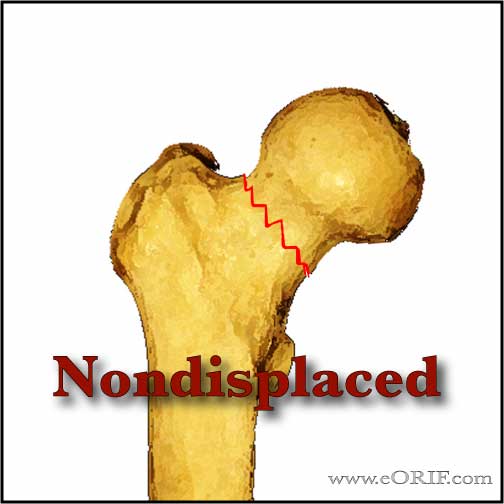
- Non-displaced (Garden 1 &2): Rx= in-situ parallel screw fixation. C-arm, cannulated screw set, supine on fx table. Place guide pin in center-center location. 3 screws total, insignificant mechanical advantage to adding more implants.
- Displaced, Young active patient (Garden III & IV): treatment = closed reduction and internal fixation. Fixation is generally performed with 3 parallel screws. Open reduction is indicated if closed reduction is unsatisfactory. Young patients with isolated, high energy femoral neck fracture are at high risk for nonunion & AVN. (Swiontkowski MF, JBJS 1984;66A:837). Consider dynamic hip screw with derotational screw for vertical or severely comminuted fractures. 25% nonunion risk(Rx-valgus osteotomy), 30% osteonecrosis risk(Rx=arthroplasty). Quality of reduction appears most important to avoid nonunions and osteonecrosis
- Displaced, Elderly inactive patient (Garden III & IV): treatment = primary prosthetic replacement. Hemiarthroplasty for patients without underlying arthritis; THA for patients with underlying arthritis.
-Hemiarthroplasty generally performed with a cemented modular unipolar prosthesis. The clinical benefits of bipolar designs are questionable and are generally not consider to warrant the added expense.
-Surgery should be performed ASAP after medical clearance, usually within 24-48 hours. Medical conditions should be stabilized before surgery. (Sexson SB, JOT 1988;1:298)
-Anestesia: type has not been shown to affect outcomes. (Davis FM, Br J Anaesth 1987;59:1080)
-CRPP vs Replacement; patients >70 years old displaced femoral neck fracture: 45.6% failure after internal fixation; 8.8% after Replacement. The rate of mortality was high at 75% at ten years, and was the same in both groups at all times. Successfully healed fractures never attained a better outcome regarding pain or function. (Leonardsson O, J Bone Joint Surg Br 2010;92(3):406-412).
- Basicercival Femoral Neck Fracture: fractures located just proximal to or at the intertrochanteric line.
-Treatment: DHSwith superior antirotation screw.
- The difference between "young active" and "elderly inactive" is not an exact age or activity level, but rather the surgeons judgement of the patients bone density and preinjury physical function.
- Non-operative management results in unacceptably high rates of medical morbidity, mortality, malunion and nonunion. May consider for elderly demented patients who were nonambulators prior to injury and who experience minimal discomfort. Patients should be mobilized ASAP to reduce the risks of decubitus ulcers, urinary tract infections, DVT/PE and atelectasis.
- Buck's skin traction has not been shown to be beneficial (Anderson GH, JBJS 1993;75Br:794). If used do not use >5 lbs. Traction must be removed and skin fully evaluated frequently to avoid complications.
- Elderly pts with fragility fractures should be evaluated for osteoporosis.
- AO Classification. AO Classification
- Garden classification: generally not used in clinical decision making. Grade I = incomplete or valgus impacted fracture. Grade II = complete fracture without displacement of the fracture fragments. Grade III = complete fracture with partial displacement of fracture fragments. Grade IV = complete fracture with total displacement of the fracture fragments, allowing the femoral head to rotate back to an anatomic position.
Femoral Neck Fracture Associated Injuries
- Elderly=head injury(subdural/epidural hematoma), distal radius, proximal humerus fx. More common to have CVA or myocardial infarction responsible for the fall
- Femoral Neck-Shaft Fracture
Femoral Neck Fracture Complications
- Nondisplaced fracture = nonunion<5%, osteonecrosis<10%
- Displaced fracture = nonunion-10-30%, osteonecrosis=15-33% c internal fixation (Koval KJ, JAAOS 1994;2:141).
- Loss of fixation / fixation failure: increased risk with increased initial displacement, non-anatomic reduction, increased patient age, and posterior femoral-neck comminution.
- Nonunion: Elderly patients can be treated with conversion to THA or hemiarthroplasty, consider using long-stemmed implant, or revision modular THA system to provide stem lengths long enough to get past any screw holes left from previous fixation. Young patients can be treated with valgus osteotomy, =+/- bone grafting, and muscle-pedicle grafting (Marti RK, JBJS 1989;71Br:782)
- Infection
- Dislocation
- Decubitus ulcers
- Urinary tract infections
- Deep venous thrombosis and pulmonary complications
- Subtrochanteric fracture
Femoral Neck Fracture Follow up care
- Post-op: WBAT. DVT prophylaxis is indicated.
-Time to functional return is faster for patients who are allowed to weight bear early, presumably because those patients unable to maintain a strict non weight bearing status are left in bed for extended periods of time. (Koval KJ, JBJS 1998A;80:357).
-Cognitively intact elderly patients with no other significant comorbidities, stable fracture patterns, and a well placed fixation device should be allowed to be either partially or fully weight bearing within 24-36 hrs after surgery.
-No study has shown immediate weight bearing to contribute to mechanical failure of the implant, however several studies demonstrate that the muscle forces across the hip joint required to maintain a strict non weight bearing status are greater than those with partial or full weight bearing.
-Elderly pts with fragility fractures should be evaluated for osteoporosis.
- 7-10 Days: Wound check, eval reduction on xrays.
- 6 Weeks: Evaluate reduction / fracture union / consolidation on xrays.
- 3 Months:Evaluate reduction / fracture union / consolidation on xrays.
- 6 Months:Evaluate reduction / fracture union / consolidation on xrays.
- 1Yr: Assess outcomes, evaluated xrays for posttraumatic osteonecrosis.
- 2Yr: Assess outcomes, evaluated xrays for posttraumatic osteonecrosis.
- 3Yr: Assess outcomes, evaluated xrays for posttraumatic osteonecrosis.
- After hip fracture the vast majority of patients require assistance in performing ADLs. Only 20% to 35% of patients who were independent in ADLs before fracture will regain their prefracture ADL independence. Factors predictive of recovery of function in ADL are younger age, absence of dementia or delirium in nondemented patients, and a strong social network. (Koval KJ, JAAOS 1994;2:141).
Femoral Neck Fracture Review References
- Rockwood and Greens
- Probe R, JAAOS 2006;14:565
- Koval KJ, JAAOS 1994;2:141
- Swiontkowski MF, Winquist RA, Hansen ST Jr. Fractures of the femoral neck in patients between the ages of twelve and forty-nine years. J Bone Joint Surg Am. 1984 Jul;66(6):837-46. PubMed PMID: 6736085.
- Haidukewych GJ, Rothwell WS, Jacofsky DJ, Torchia ME, Berry DJ. Operative treatment of femoral neck fractures in patients between the ages of fifteen and fifty years. J Bone Joint Surg Am. 2004 Aug;86-A(8):1711-6. PubMed PMID: 15292419.
- Upadhyay A, Jain P, Mishra P, Maini L, Gautum VK, Dhaon BK. Delayed internal fixation of fractures of the neck of the femur in young adults. A prospective, randomised study comparing closed and open reduction. J Bone Joint Surg Br. 2004 Sep;86(7):1035-40. PubMed PMID:15446534.
- Nowotarski PJ, Ervin B, Weatherby B, Pettit J, Goulet R, Norris B.Biomechanical analysis of a novel femoral neck locking plate for treatment of vertical shear Pauwel's type C femoral neck fractures. Injury. 2012 Jun;43(6):802-6. doi: 10.1016/j.injury.2011.09.012. Epub 2011 Oct 21. PubMed PMID: 15446534.
|