|

|
synonyms: Panner’s Disease, osteochondritis dessicans of the capitellum, capitellar OCD, Little League Elbow, Little Leaguer's Elbow
Capitellar OCD ICD-10
Capitellar OCD ICD-9
- 732.3 (juvenile osteochondrosis of the upper extremity, includes capitellum of humerus and others)
Capitellar OCD Etiology / Epidemiology / Natural History
- Occurs in adolescent athletes who place valgus compressive stress on the elbow.
- Generally baseball pitchers age 13-15 years old; Gymnasts.
- Panner's disease is a juvenile osteochondrosis of the capitellum occuring in patients aged 7-12y/o, generally boys. Xrays demonstrate fragmentation (not collapse) of the capitellar epiphysis and flattening and patchy sclerosis of the capitellum.
- Etiology: repetitive valgus overloads causing compression at the radiocapitellar joint with subsequent subcondral microtrauma/microfracture, tenous vascular supply to the capitellum, mechanical mismatch between the stiffer radial head articular cartilage and the soft capittelar cartilage, genetic predispostion.
- <10% of gymnasts with Capitellar OCD will be able to return to sport. (Maffuli N, JPO, 1992;12:344).
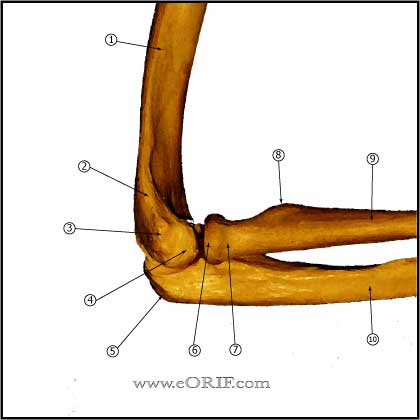
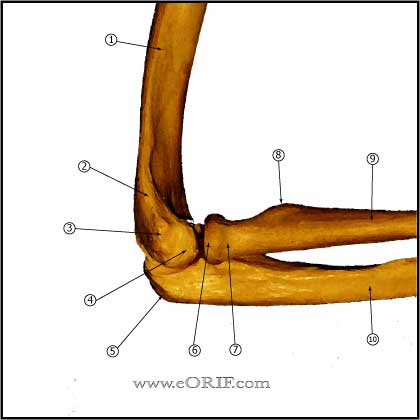
Capitellar OCD Anatomy
- The capitellar epiphysis has a tenous blood supply consisting of 2 vessels which enter posteriorly and transverse the cartilaginous capitellum. (Haraldson S, Acta Orthop Scand 1959;38sup 1-232). Radial recurrent and interosseous recurrent arteries.
- Capitellar articular cartilage is significantly softer than that of the radial head which may contibute to the developement of capittelar OCD, (Schenk RJ, CORR 1994;299:305).
- See also Elbow Anatomy.
Capitellar OCD Clinical Evaluation
- Activity related posterolateral elbow pain +/- swelling and decreased ROM. May note popping / locking if loose body is present.
- Evaluate ROM, locking, loss of full extension may be assoicated with loose body.
- Tenderness along radiocapitellar joint.
- Active Radiocapitellar Compression Test: patient pronates and supinates the forearm in full extension causing compression at the radiocapitellar joint. Positive test: reproduction of patient's symptoms.
Capitellar OCD Xray / Diagnositc Tests
- A/P, lateral and oblique elbow films indicated. Evaluate for capitellar irregularities and loose bodies. Early changes include subtle rarefraction, and flattening in the posterolateral capitellum. Consider getting comparison views of the normal elbow.
- MRI: Helpful to define extent of OCD and provide definitive diagnosis in early cases. Earliest changes = low signal changes in the superficial aspect of the capitellum on T1 images; T2 images may be normal (Takahara M, JBJS 1998;80A:892).
Capitellar OCD Classification / Treatment
- Grade I: translucent cystic changes in the posterolateral capitellum without evidence of subchondral collapse. Ia= no loss of subchondral stability. Ib= unstable subchondral bone with impending collapse: intitially treated non-operatively (Takahara M, AJSM 1999;27:728).
- Grade II; clear zone or fracture line between the lesion and the adjacent subchondral bone (subchondral collapse): intitially treated non-operatively.
- Grade III: detached osteochondral fragments / intraarticular loose bodies. Treatment: elbow arthroscopy with loose body removal and microfracture (Baumgarten TE, AJSM 1998;26:520), Byrd JW, AJSM 2002;30:474). May consider fragment fixation with bone graft (Harada M, JSES 2002;11:368), or autologous chondrocyte implantation.
- Non-operative: activity restriction/modification of sports activitys until symptoms resolve. Consider offloading double-hinged elbow brace: ROM set to painfree limits, NSAIDs for pain, brace worn at all times initially, continue brace until xrays demonstrate healing, usually 12-16 weeks, may play sports in brace as long as elbow is painfree. PT protocol includes: flexor/pronator strengthening, RTC strengthening, wrist ROM/strengthening, wall push-ups, bicep curls and tricep pushdowns; all done with brace on.
- Operative: indicated for any sign of loose body(loss of full extension/locking) Surgery = Elbow Arthroscopy with debridement/loose body removal, microfracture of the defect may be useful. Consider fixation of any large osteochondral fragments.
- Panner's Disease treatment rest, activity modifications. Disease is self-limiting.
Capitellar OCD Associated Injuries / Differential Diagnosis
Elbow Scope Complications
- 11% minor complications, 0.8% major (Kelley EW, JBJS 2001;83A:25).
- Overall approximately 10% complication rate
- Compartment syndrome
- Septic arthritis / infection: 0.8% (Kelley EW, JBJS 2001;83A:25).
- Nerve injury (median, ulnar, radial, posterior interosseous): use of retractors effectively decreases risk.
- Cutneous neuromas (associated with portal placement).
- 4%transient radial-nerve palsy after intraarticular anesthetic injection
- Vascular injury
- Prolonged drainage (portal sites): 4% aseptic drainage
- Stiffness / flexion contracture
Capitellar OCD Follow-up Care
- Post Op: double-hinged elbow brace: ROM 30° to full flexion.
- 7-10 Days: brace worn at all times initially. Start PT focused on ROM.
- 6 Weeks: continue brace until xrays demonstrate healing, usually 12-16 weeks.
- 3 Months: may play sports in brace as long as elbow is painfree. PT protocol includes: flexor/pronator strengthening, RTC strengthening, wrist ROM/strengthening, wall push-ups, bicep curls and tricep pushdowns; all done with brace on.
- 70-82% of patients treated surgically return to previous level of activity (Baumgarten TE, AJSM 1998;26:520).
- <10% of gymnasts with Capitellar OCD will be able to return to sport. (Maffuli N, JPO, 1992;12:344).
Capitellar OCD Review References
- Kobayashi K, JAAOS 2004;12:246
- Yadao MA, ICL 2004;53:599
- Schenck RC Jr, JBJS 1996;78A:439
- Peterson R, ICL 1999;48:393.
- Takahara M, CORR, 1999;363:108
|