|
|
Spinal Cord Injury ICD-10
- S14.109A Unspecified injury at unspecified level of cervical spinal cord, initial encounter
- S24.109A Unspecified injury at unspecified level of thoracic spinal cord, initial encounter
- S34.109A Unspecified injury to unspecified level of lumbar spinal cord, initial encounter
- See all Spinal Cord Injury ICD-10
Spinal Cord Injury ICD-9
- 952 Spinal cord injury without evidence of spinal bone injury
Synonyms: spinal cord injury, SCI,
Spinal Cord Injury Etiology / Epidemiology / Natural History
- Caused by penetrating trauma / violence, MVA, falls, sports injury
- Average age =32, 81% male.
- Shortened life expectancy generally related to pulmonary complications.
- Neurologic deficits are determined by primary and secondary (oxygen free radicals, calcium homeostasis disruption, opiate receptor abnormalities,, lipid peroxidation and excitatory neurotrasmitter acculumation [glutamate]) injurys.
- Paralytic scoliosis will develops in nearly 100% of children with complete cervical cord injuries before age 10 (Dearolf WW III, LPO 1990;10:214).
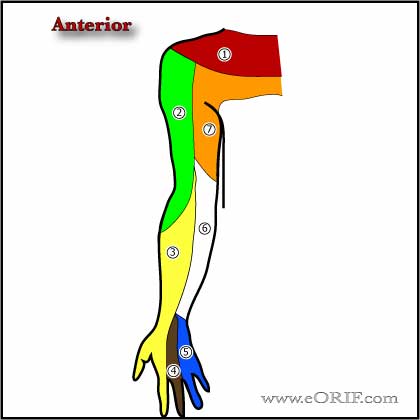
Spinal Cord Injury Anatomy
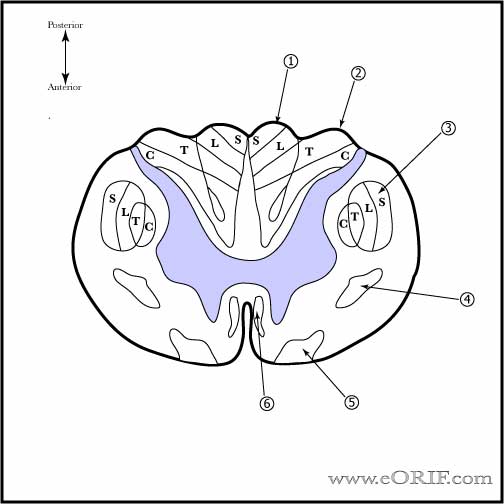
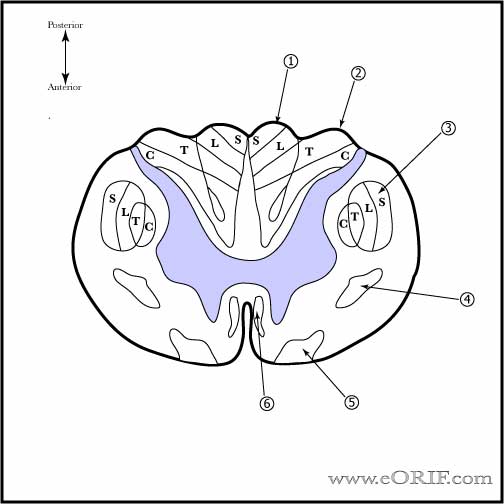
- Dorsal Column:ascending tract containing proprioception, vibratory sense, discriminative touch
- Spinothalamic tract: ascending tract containing paiin, crude temperature, light touch
- Spinocerebellar tract: ascending tract containing subconscious regulation of muscle position and tone
- Corticospinl tract: descending tract containing voluntary motor function
- Rubrospinal tract: descending tract containing felxor muscle tone control
- Vestibulospinal tract:descending tract containing spinal cord relexes and muscle tone regulation
- Reticulospinal tract: descending tract containing influences voluntary movement, head position and muscle tone
Spinal Cord Injury Clinical Evaluation
- ATLS exam, compete neurologic exam, Spinal shock: can mimic complete SCI. Lasts 24-48 hours. Return of bulbocanvernosus relex indicates end of spinal shock. Level of spinal injury can not be determined until bulbocaverosus reflex has returned.
- Use ASIA exam sheet.
Spinal Cord Injury Xray / Diagnositc Tests
- Lateral c-spine generally taken as part of ATLS. CT cervical spine: indicated for obtunded patients before c-spine clearance.
- Plain films: xrays of entire spine due to high incidence of non-contiguous injuries (Keenen TL, J Trauma 1990;30:489).
- CT +/- MRI generally indicated.
- MRI: pre-reduction MRI remains controversial. Reduction should not be significantly delayed for MRI. (Darsaut TE, Spine 2006;31:2085).
Spinal Cord Injury Classification
Complete SCI: comlete loss of all motor and sensory function below the level of injury, poor prognosis.
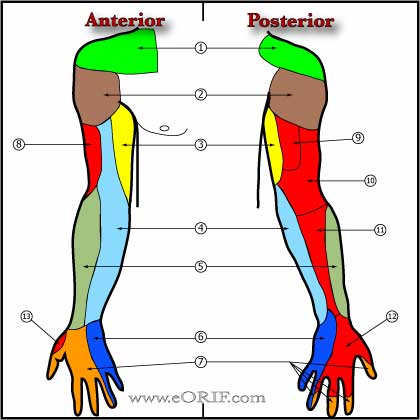
- C1-C3: ventilator dependent, limited talking ability. Head or chin control wheelchair. Needs assistance for transfers, ADL's.
- C3-C4: Can become ventilator independent. Head or chin control wheelchair. Needs assistance for transfers, ADL's.
- C5: ventilator independent, biceps/deltoid funtion, independent in ADLs. Head or chin control wheelchair. Limited mobility hand control wheelchair. Needs assistance with transfers/living.
- C6: Wrist flexion/extension, independent ADL's/living. Hand control wheelchair, can drive hand control car. May need assistance with transfers.
- C7: Triceps. Manual wheelchair capable, can drive hand control car, independent ADL's/living. May need assistance with transfers
- C8-T1: Hand/finger dexterity. Independent transfers/ADL's/living, manual wheelchair, can drive hand control car.
- T2-T6: Normal upper extremity function, some trunk control. Independent transfers/ADL's/Living, manual wheelchair, can drive hand control car.
- T7-T12: Unsupported sitting ability. Independent transfers/ADL's/Living, manual wheelchair, can drive hand control car, walking possible with extensive bracing.
- L1-L5: variable lower extremity/bowel/bladder funtion. Independent transfers/ADL's/Living, manual wheelchair, can drive hand control car, walking possible with bracing.
- S1-S5: variable bowel/bladder/sexual function. Independent
Incomplete SCI: partial motor or sensory loss below the level of injury.
- Central Cord Syndrome: most common; generally older patients with underlying spinal stenosis. Hyperextension injury. Greater weakness in the upper extremities and lower extremities. Favorable prognosis.
- Anterior Cord Syndrome: generally from vascular insult, HNP, vertebral body fracture. Motor , light touch and pain sensation impaired. Deep pressure, proprioception and vibration intact. Poor prognosis for functional improvement.
- Posterior-Cord Syndrome: proprioception, deep pressure and vibration impaired. Motor funtion normal. Rare
- Brown-Sequard Sydrome: motor and proprioception on ipsilateral side of injury impaired; pain and temperature on contralateral side impaired. Generally from penetrating trauma. Favorable prognosis for functional recovery.
- Conus medullaris syndrome: injury to the sacral cord and lumbar nerve roots leading to areflexic bladder, bowel, and lower limbs. Sacral segments occasionally show preserved reflexes (bulbocavernosus and micturition reflexes).
- Cauda equina syndrome: injury to the lumbosacral nerve roots in the spinal canal leading to areflexic bladder, bowel, and lower limbs
Spinal Cord Injury Acute Treatment
- ATLS Protocol.
- Any trauma pt with suspected C-spine injury should be immobilized on a spine board with cervical collar and log-roll precautions until the c-spine has been cleared.
- Maintain oxygen saturation >96%. 100% oxygen via nasal cannula, intubation may be required for upper cervical lesions.
- Maintain systolic BP >90mmHg. Neurogenic shock: Heart rate typically 50-70 beats per minute; SBP 30-50 mm Hg below normal. Must be differentiated from hypovolemic shock(tachycardia/hyptotension). Treatment =initial fluid challenge,Trendelenburg positioning, central line placement, vasopressors (dopamine/phenylephrine hydrochloride), atropine for bradyarrhythmia.
- Cervical tractionwith tongs or a halo ring indicated for neurologic deficit or evidence of cervical spine instability. Contraindications= cervical distraction injuries at any level, type IIA hangman's fractures.
- Surgery indicated for neural compression and neruologic deterioration/deficit and spinal instability. Consider surgery for residual cord compression without deficit.
- Methylprednisolone bolus dose 30 mg/kg followed by 5.4 mg/kg per hour for 23hours if given withing the first 3 hours of injury. If given 3 to 8 hrs after injury continue for 48 hours. Do not give if >8hrs from injury. (Bracken MB, JAMA 1997;277:1597). Steriod administration for spinal cord injury is currently controversial and is associated with higher risks for pneuonia, pulmonary embolism and wound infection/sepsis and has not been studied for penetrating injuries.
- Future Considerations: Minocycline, erythropoietin, olfactor ensheathing cells (Baptiste DC, J Neurotrauma 2006;23:318).
Spinal Cord Injury Associated Injuries / Differential Diagnosis
- Fractures
- Pneumothorax/hemothorax
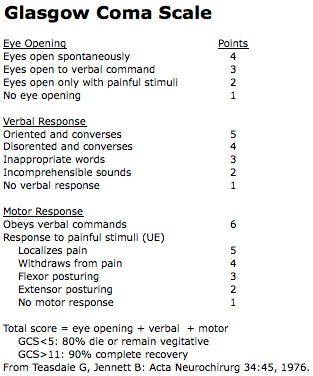
- Head injury
Spinal Cord Injury Complications
- Skin Breakdown
- Autonomic dysreflexia
- Osteoporosis / Fractures
- Pneumonia, atelectasis, aspiration
- Heterotopic ossification
- Spasticity
- DVT
- Cardivascular disease
- Syringomyelia
- Neuropathic pain
Spinal Cord Injury Follow-up Care
- 92% discharged to independent living or residential living with assistance.
- Patient information: www.spinalinjury.net.
Spinal Cord Injury Review References
|