|





|
synonyms: TSA, total shoulder arthroplasty, total shoulder replacement, shoulder hemiarthroplasty
Shoulder Arthroplasty CPT
Shoulder Arthroplasty ICD-10 Codes
- M19.011 - Primary osteoarthritis, right shoulder
- M19.012 - Primary osteoarthritis, left shoulder
- M19.019 - Primary osteoarthritis, unspecified shoulder
- Z47.1 - Aftercare following joint replacement surgery
- Z47.31 - Aftercare following explantation of shoulder joint prosthesis
- Z96.61 - Presence of artificial shoulder joint
- Z96.611 - Presence of right artificial shoulder joint
- Z96.612 - Presence of left artificial shoulder joint
Shoulder Arthroplasty Indications
- Pain from an incongruous joint associated with end-stage glenohumeral arthritis that has failed non-operative management
- Glenohumeral arthritis may be caused by osteoarthritis, avascular necrosis, capsulorraphy arthropathy, dislocation arthropathy, rheumatoid arthritis (Trail IA, JBJS 2002;84Br:1121), instability surgery (Sperling JW, JBJS 2002;84A:1775).
- Hemiarthroplasty indications: early ostenoecrosis before glenoid changes; severe glenoid bone loss, rotator cuff arthropathy.
TSA Contraindications
TSA Alternatives
- Non-operative care: NSAID's, activity modifications, glenohumeral steriod injection
- Arthroscopic debridement (consider for young patients with concentric glenoid wear, minimal bone loss, absence of contracture, loose bodies).
- Shoulder Arthrodesis
- Hemiarthroplasty: TSA demonstrates improved pain relief, hemiarthroplasty has potential need for revision to TSA. (Gartsman GM, JBJS 2000;82A:26). High rate of unsatisfactory results with frequent need for revision (Rispoli DM, JBJS 2006;88A:2637)
- Interposition arthroplasty: with or without hemiarthroplasty. Graft options: anterior capsule, fascia lata, achilles allograft, lateral meniscal allograft, dura mater, porcine submucosa. 50% excellent, 36% satisfactory, 14% unsatisfactory for biologic glenoid resurfacing with hemiarthroplasty (Kirshnan SG, JBJS 2007;89A:727).
TSA Pre-op Planning / Special Considerations
- Principles: restore soft tissue balance, version, and joint stability
- Obtain ESR, CRP and consider asperation with aneorobic, aerobic, fungal and acid-fast bacterial cultures in patients with history of prior surgery.
- Glenoid Considerations
- Humeral Considerations
- Concomitant biceps tenotomy has demonstrated improved outcomes at 1 yr post-op (Simmen BR, JSES 2008;17:921).
- Xrays
- Parkinson's disease: patients with Parkinson's have been shown to have increased risk of instability and marginal outcomes with TSA. 47% unsatisfactory results. (Kryzak TJ, JSES 2009;18:96).
- Prior mastectomy / history of lymphedema: Patients with prior history of lymphedema, or history of mastectomy have increased risk of lymphedema after TSA and may have higher risk of infection and shoulder stiffness. Lymphedema can be managed by occupational therapist generally using compression sleeves. Best managed in a specialized lymphedema clinic.
Shoulder Arthroplasty Peri-operative Pain Protocol
- 10 mg dexamethasone IV within 90 minutes of surgery.
- Intraoperative 62-mL local infiltration cocktail: 300 mg (60 mL) 0.5% ropivacaine, 30 mg (1 mL) ketorolac, and 10 mg (1 mL) epinephrine.
- First 24 hours postop
- Acetaminophen 975 mg PO every 8 hours
- Oxycodone 5-10 mg PO Q4hrs as needed for severe pain
- Meloxicam 7.5 mg PO every 6 hours
- Gabapentin 100 mg PO every 12 hours
- Diazepam 5 mg PO PRN for muscle spasms.
- Ondansetron 4mg IV Q4-6 hours as needed for nausea/vomiting.
- References: Klag E, JSES 2021;30:1544-1552
- Consider methylprednisolone (Medrol) 6 day taper. (Wagner, ER, JSES 2024:33:985-994)
Glenoid Considerations
- Glenoid Anatomy
- Glenoid resurfacing indications: (Rodosdiy MN, JSES 1996;5:231)
- Pain relief is more likely following glenoid resurfacing than hemiarthroplasty alone. (Gartsman GM, JSES 1997;6:333)
- The younger and more active a patient is the more glenoid looseing is a concern and hemiarthroplasty is a strong consideration.
- Posterior bone loss is frequently encountered and can be managed by reaming the anterior glenoid to restore anatomic version, posterior glenoid bone grafting, using an augmented glenoid component, or performing hemiarthroplasty alone. Anterior reaming causes A/P glenoid narrowing. Reaming >15º may lead to peg penetration and inability to seat glenoid (Gillespie R, Orthopaedics 2009;32:21).
- Perfect congruency between the glenoid face and the glenoid component with meticulous cementing into a dry glenoid is a must.
- Cemented all polyethylene components are the current gold standard. Current US FDA guidelines require methymethacrylate for glenoid fixation.
- Metal backed glenoid components have been associated with high failure rates and are generally not used.
- Advantages to resurfacing: less pain, less GH friction, better fulcrum, increased stability, improved strength
- Disadvantages to resurfacing: increased risk of component failure, increased surgical time, increased blood loss.
- Larger glenoid component sizes produce modest increases in stability (Tammachote N, JSES 2007;16:102S).
Humeral Component Considerations
- Humeral Head Anatomy
- Cement is unnecessary if there is immediate and substantial axial and rotational stability at the time of humeral component placement.
- Cement is indicated for patients with poor bone stock / large degenerative cysts.
Keys to Glenoid Exposure in Total Shoulder Arthroplasty
- Deltoid mobilization
- Complete inferior capsular release around humeral neck.
- Cut humeral head at Rotator cuff insertion
- Remove osteophytes around humeral head. The more narrow the humerus, the more easy the glenoid exposure.
- Slight forward elevation and internal rotation of humerus to allow humeral head to fall posteriorly.
- Remove labrum.
- Identify inferior glenoid.
- Hypotensive anesthesia and muscle relaxation.
TSA Xrays
- A/P of glenohumeral joint (Grashe view), scapula lateral and axillary views
- humeral osteophytes, humeral head flattening, irregular/narrowed joint space, subchondral cystic changes in humeral head. Acromiohumeral interval: average = 10.5mm. <7mm=full-thickness RTC tear. Measure on Grashey view. (Cotty P, J Radiol 1988;16:633).
- Evaluate axillary view for asymmetric glenoid wear and subluxation of humeral head. (Usually posterior)
- CT scan is indicated if there is any concern for posterior glenoid wear for pre-operative planning (may need glenoid bone graft). (Friedman RJ, JBJS 1992;74A:1032). Glenoid version is determined on the first transverse inferior image in which the tip of the coracoid is no longer visible.
- Subluxation Index: (Walch G, Acta Orthop Belg 1998;64suppl2:48)
- MRI is indicated if there is any concern for rotator cuff pathology (acromiohumeral interval <7mm. <5% of patients with GH arthritis has assoiated RTC tears.
- EMG is indicated if there is any concern for nerve damage.
TSA Technique
- Interscalene block with general anesthesia
- Pre-operative antibiotic
- Beach-chair position; all bony prominences well padded.
- Exam under anesthesia: if external rotations is <40 degrees strongly consider capsular release and subscapularis lengthening. In a humerus of average size, advancing the subscapularis insertion by 1cm results in 20 degrees of increased external rotation.
- Arm supported on height-adjustable Mayo stand, or shoulder positioner.
- Prep and drap affected extremity
- Deltopectoral incision from just medial to AC joint to just lateral to the proximal edge of the biceps muscle belly.
- Identify deltopectoral interval (interval can be found by palpating medial edge of deltoid insertion into clavicle or finding fat layer in interval surrounding cephalic vein.)
- Preserve cephalic vein by ligating any branches to deltoid and taking the cephalic vein and its surrounding tissues medially.
- Incise clavipectoral fascia adjacent to the conjoined tendon up to the coracoacromial ligament.
- Release upper 1/3 of pectoralis tendon if needed for exposure.
- Cauterize the anterior humeral circumflex vessels as needed.
- Tenodes the long-head of the biceps tendon to surrounding soft tissues. (Godeneche A, JSES 2002;11:11).
- Release subscapularis and anterior capsule as one unit 2cm from the lesser tuberosity insertion. Ensure long-head of biceps tendon is not injured in the proximal aspects of the release.
- Incise rotator interval medially to the level of the coracoid process.
- Tag subscapularis with sutures.
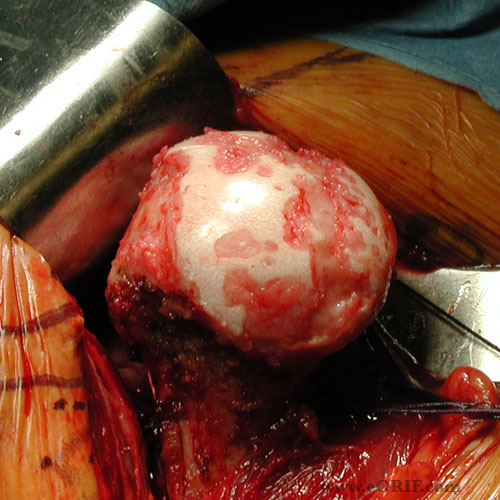
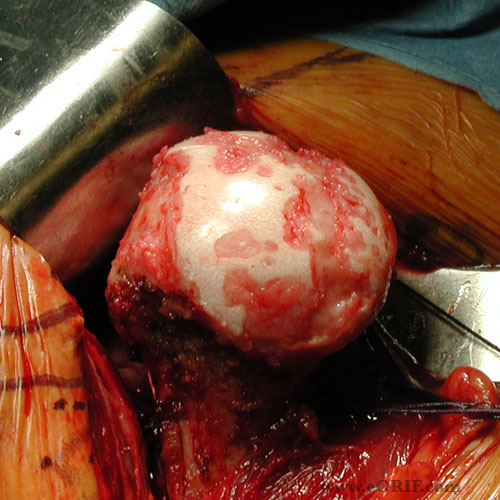
- Dislocate humeral head by hyperextending, extending and externally rotating arm.
- Remove marginal osteophytes.
- Use trocar tipped reamer to make starter hole just posterior to the bicipital groove.
- Sequentially hand ream proximal humerus in 1mm increments until cortical contact is felt.
- Leave last reamer in place
- Place humeral head cutting guide and pin in place. Remove IM reamer.
- Resect humeral head along the articular surface with saw at 30 degrees retroversion.
- Insert trial stem.
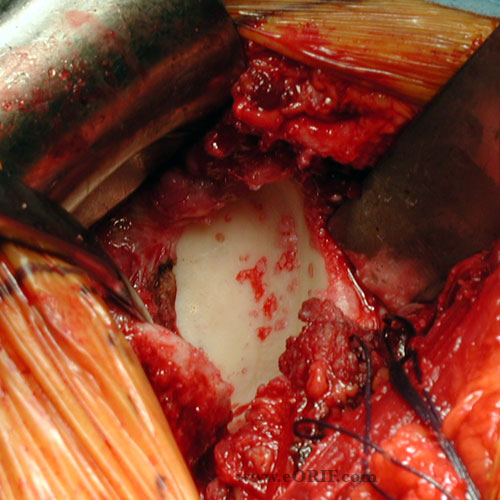
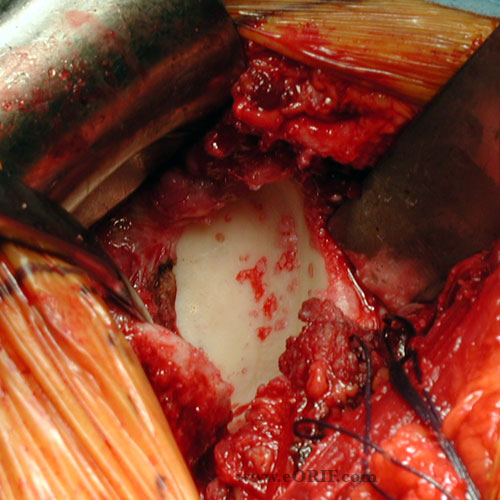
- Expose glenoid. Ensure anterior capsule is released from glenoid rim from superior to inferior and the entire neck of the glenoid can be palpated to ensure adequate exposure.
- Excise glenoid labrum.
- Evaluate bony architecture of glenoid. Especially look for posterior glenoid wear.
- Posterior glenoid wear can be corrected by: Reaming down the anterior glenoid to match the posterior wear; bone graft the posterior glenoid; using a posteriorly augment glenoid component. (Hill JM, JBJS 2001;83A:877).
- Remove remaining glenoid cartilage with a glenoid scaper/planer.
- Size glenoid.
- Drill centering hole.
- Ream glenoid surface.
- Prepare glenoid keel or peg holes.
- Place trial components and ensure anatomic fit.
- Irrigate.
- Close in layers.
TSA Complications
- Overall 12% incidence (Chin PY, JSES, 2006;15:19), (14%=Cofield RH, ICL 1990;39:449).
- Instability / soft tissue imbalance:
- Rotator cuff tear (Hattrup SJ, JSES, 2006;15:78).
- Ectopic ossification
- Glenoid loosening: consider revision if symptomatic (Antuna SA, JSES 2001;10:217).
- Peri-Prosthetic fracture (0.5%-3%)
- Nerve injury (Lynch NM, JSES 1996;5:53).
- Periprosthetic Infection: <1% with peri-operative antibiotics
- Humeral loosening
- Long-head of biceps rupture
- 52% of patients of TSA patients travelling domestically will activate security gates. 42% traveling internationally. (Dines JS, JSES 2007;16:434).
- Pulmonary Embolism: <.5% (Sperling JW, JBJS 2002;84A:1939)
TSA Follow-up care
TSA Outcomes
TSA Review References
|