|
|
synonyms: scapular body fracture, scapula fracture
Scapula Fx ICD-10
- S42.109A - Fracture of unspecified part of scapula, unspecified shoulder, initial encounter for closed fracture
- S42.111A - Displaced fracture of body of scapula, right shoulder, initial encounter for closed fracture
- S42.112A - Displaced fracture of body of scapula, left shoulder, initial encounter for closed fracture
- S42.113A - Displaced fracture of body of scapula, unspecified shoulder, initial encounter for closed fracture
- S42.114A - Nondisplaced fracture of body of scapula, right shoulder, initial encounter for closed fracture
- S42.115A - Nondisplaced fracture of body of scapula, left shoulder, initial encounter for closed fracture
- S42.116A - Nondisplaced fracture of body of scapula, unspecified shoulder, initial encounter for closed fracture
- See all Body Scapula fracture ICD-10.
A - initial encounter for closed fracture
B - initial encounter for open fracture
D - subsequent encounter for fracture with routine healing
G - subsequent encounter for fracture with delayed healing
K - subsequent encounter for fracture with nonunion
P - subsequent encounter for fracture with malunion
S - sequela
Scapula Fx ICD-9
- 811.00 (fracture of scapula, upper end, unspecifiec part, closed)
- 811.09 (fracture of other parts of scapula, closed)
Scapula Fx Etiology / Epidemiology / Natural History
- Uncommon injury.
- Generally high-energy direct blow to the posterior shoulder.
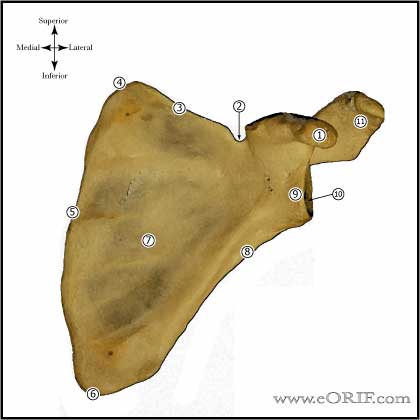
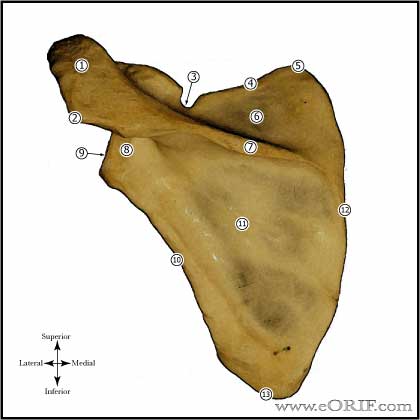
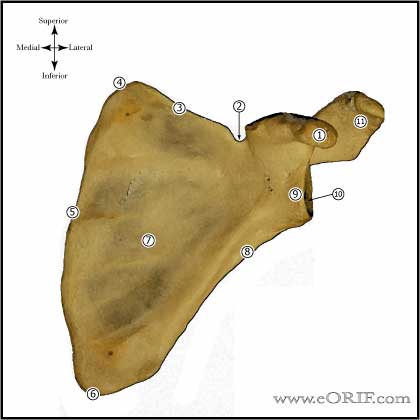
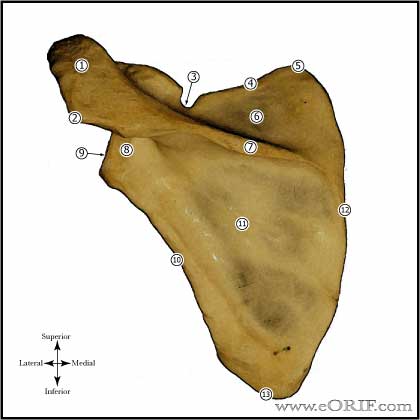
Scapula Fx Anatomy
Scapula Fx Clinical Evaluation
- ATLS resuscitation. These are typically high enegery injuries, assessment should begins with the A,B,C's.
- C/O shoulder pain after trauma.
- Evaluate for tenderness, ecchymosis, soft tissue injury.
- Document axillary, median, ulnar, radial nerve function and radial pulse.
Scapula Fx Xray / Diagnositc Tests
- AP, scapular lateral and axillaryviews.
- CT scan with 2-3mm cuts often helpful to fully define fracture pattern.
- Consider Chest xray to rule out associated injuries.
Scapula Fx Classification / Treatment
- Location: Scapular body, glenoid neck, glenoid fossa, coracoid process, acromion.
- 68% involve the inferior aspect of the glenoid neck, 71% involve the superior vertebral border (Armitage BM, JBJS 2009;91A:2222).
- Scapular body fractures are generally treated conservatively.
- Operative indications: greater than 20mm medial/lateral displacement of the glenohumeral joint, medialiazation of the glenohumeral joint relative to the lateral boarder of the scapula, greater then 45º of angular deformity in the semicoronal plane, angulation greater than 30º and medialization greater then 15mm, double disruption of the superior shoulder suspensory complex displaced greater than 10mm, open fracture, glenopolar angle less than 22º (GPA=angle formed by lines connecting the inferior glenoid to the superior glenoid to the inferior angle of the scapula)
- ORIF technique: generally utilize Judet apporach with skin incision paralleling the spine of the scapula and medial border of the scapula. Deltoid is detached from scapular spine. Infraspinatus reflected laterally exposing scapular body.
Scapula Fx Associated Injuries / Differential Diagnosis
Scapula Fx Complications
- Nonunion
- Malunion
- Infection
- Neurovascular Injury
- Pneumothorax
- Brachial plexus injury
Scapula Fx Follow-up Care
- Post-op: sling for comfort, no overhead motion. Immediate pendelum ROM exercises.
- 10-14 Days: Wound check, sutures removed. Start PT for gentle ROM exercises. No resistive exercises/activities. Sling as needed for comfort.
- 6 weeks: Xrays, if union is evident begin strengthening and resistive exercises. No contant athletics.
- 3 months: Repeat xrays. If pt is painfree and union is obvious pt may return to sport.
- 22% fair/poor results at 10-20 year f/u with non-op treatment (Nordqvist A, CORR 1992;283:139).
- Shoulder Outcome measures.
Scapula Fx Review References
- Thompson DA, Flynn TC, Miller PW, et al: The significance of scapular fractures. JOT 1985;25:974-977.
- Orthopaedic Knowledge Update: Shoulder and Elbow, No. 3, 2008

- Warner JP, Complex and Revision Problems in Shoulder Surgery, 2005
|