|



|
synonyms: coal miner's elbow, student's elbow
Olecranon Bursitis ICD-10
Olecranon Bursitis ICD-9
- 726.33 (olecranon bursitis)
Olecranon Bursitis Etiology / Epidemiology / Natural History
- Definition: inflammation of the olecranon bursa
- Associated with football (artificial turf), hockey, wrestling, volleyball.
- Can result from a direct blow, repetitive microtrauma, or infection
- Etiology: overuse, inflammation, infection, trauma. Idiopathic swelling due to repetitive use of the elbow or to local irritation from rubbing the elbow on some surface; Can also be due to gout, rheumatoid arthritis, pigmented villonodular synovitis
- Risk factors: alcoholsim, diabetes mellitius, hemodialysis, anticoagulants.
- Septic bursitis is most commonly caused by staph aureus.
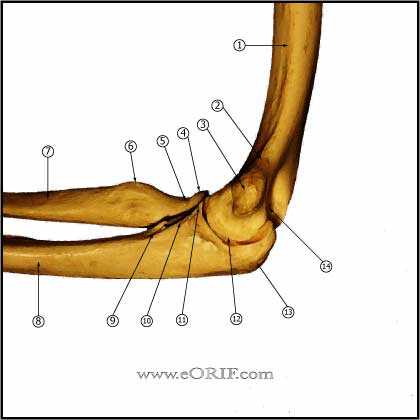
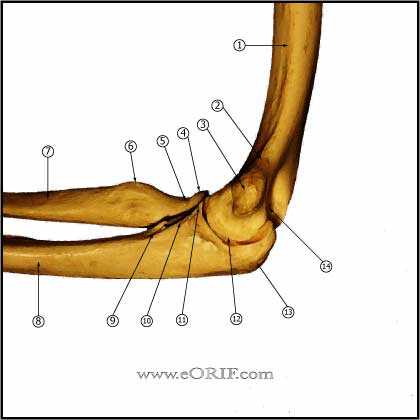
Olecranon Bursitis Anatomy
- Olecranon bursa: superficial bursa (between skin and tendon); intratendinous burse (in the substance of the tendon); subtendinous burse (between tendon and capsule). Olecranon bursitis involves the superficial bursa
Olecranon Bursitis Clinical Evaluation
- Generally painless distention of the olecranon bursa.
- Severe pain and erythema may indicate septic bursitis or gout.
Olecranon Bursitis Xray / Diagnositc Tests
Olecranon Bursitis Classification / Treatment
- Acute: ice, compressive elbow sleeve (with elbow pad to eliminate repeated trauma, Heelbo Heel / Elbow Protector), avoidance of repeated trauma to olecranon. Consider aspiration for severe swelling, or if needed to rule out septic bursitis. Aspiration risks infecting a previously sterile bursitis and the development of draining sinus tract.
- Chronic: compressive elbow sleeve (with elbow pad to eliminate repeated trauma) avoidance of repeated trauma to olecranon. Consider aspiration (CPT 20605) for severe swelling, or if needed to rule out septic bursitis. Aspiration risks infecting a previously sterile bursitis and the development of draining sinus tract. Consider surgical excision for cases refractory to non-surgical management (Stewart NJ, JSES 1997;6:49).
- Septic: diagnosis is confirmed with aspiration (send for cell count, gram stain, anaerobic & aerobic cultures, crystals. Most common organism is staph aureus (Ho G, Arch Intern Med 1979;139:1269). Treatment: needle aspiration and lavage with injection of 0.5g of methicillin in 10mL of saline followed by oral antibiotics determined by cultures and sensitivities and compressive elbow sleeve. Consider admission for IV antibiotics. Arthroscopic vs open irrigation and debridement indicated for cases which fail to improve with IV antibiotics and needle aspiration / lavage. It is best to delay surgical excision until inflammation has subsided, and skin conditions will allow surgery.
- CPT: 24105 Excision, olecranon bursa
- Olecranon Bursitis Patient Information
Olecranon Bursitis Associated Injuries / Differential Diagnosis
Olecranon Bursitis Complications
- Infection
- Skin slough
- Recurrence
Olecranon Bursitis Follow-up Care
- Recurrence is common is repetitive microtrauma is not avoided.
- Full recovery after excision may take a year.
- 94% satisfactory result of patients (15 of 16), 40% satisfactory in RA patients (Stewart NJ, JSES 1997;6:49).
Olecranon Bursitis Review References
|