|
 


|
synonyms: shoulder arthritis, Glenohumeral Arthritis, shoulder osteoarthritis, glenohumeral arthritis
Glenohumeral Arthritis ICD-10
Glenohumeral Arthritis ICD-9
- 715.11 (primary osteoarthritis, shoulder region)
- 715.21 (secondary osteoarthritis, shoulder region)
Glenohumeral Arthritis Etiology / Epidemiology / Natural History
- Glenohumeral arthritis may be caused by osteoarthritis, avascular necrosis, capsulorraphy arthropathy, dislocation arthropathy, rheumatoid arthritis, posttraumatic arthritis, septic arthritis, cuff tear arthropathy, malunion or nonunion of proximal humerus fracture.
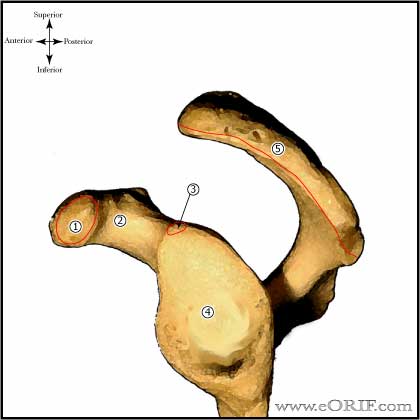
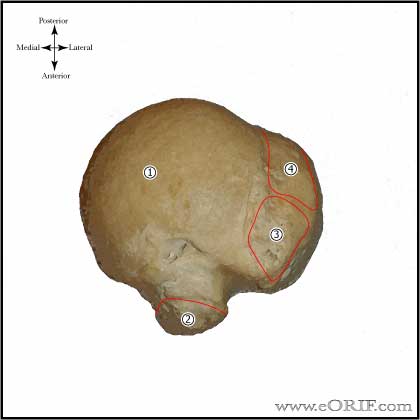
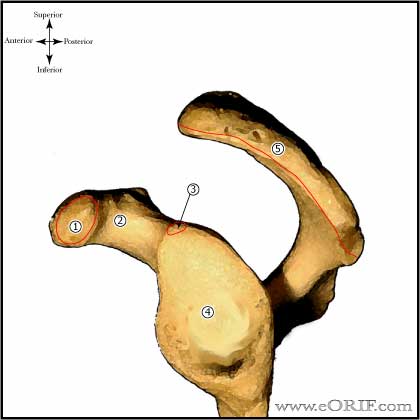
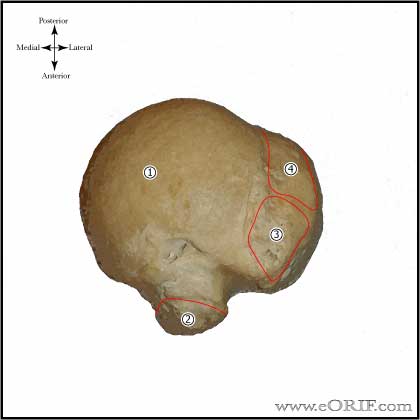
Glenohumeral Arthritis Anatomy
Glenohumeral Arthritis Clinical Evaluation
- Keys= usually >50y/o, progressive pain, rest pain, known arthritis( RA), crepitus, decreased Rom. May be in 30-40's who previously underwent instability repairs.
- Gradually progressive shoulder pain generally over several-year history
- Progessive stiffness and loss of motion. Often complain more of limited function and difficulties with ADL's than pain.
- Generally restricted passive ROM
- Generally normal strength
- May have niGlenohumeralt pain, which is generally positional and less
- C-spine exam is indicated including ROM in all planes and full neuro exam.
Glenohumeral Arthritis Xray / Diagnositc Tests
- AP, scapular lateral and axillary views.
- Primary OA demonstrates humeral osteophytes, humeral head flattening, irregular/narrowed joint space, subchondral cystic changes in humeral head and posterior glenoid wear.
- Rheumatoid arthritis demonstrates central glenoid wear, osteopenia, bone erosions, subchondral cysts, +/- osteophyte formation.
- Evaluate axillary view for asymmetric glenoid wear and subluxation of humeral head. (Usually posterior)
- Shoulder arthritis grading scales: For Dislocation arthropathy see: (Samilson RL, JBJS 1983;65Am:456-460).
- CT scan is indicated if there is any concern for posterior glenoid wear for pre-operative planning (may need glenoid bone graft). (Friedman RJ, JBJS 1992;74A:1032).
- MRI is indicated if there is any concern for rotator cuff pathology. <5% of patients with Glenohumeral arthritis has assoiated RTC tears.
- EMG is indicated if there is any concern for nerve damage.
Glenohumeral Arthritis Classification / Treatment
- Non-surgical: Education, NSAID's, activity modifications. Intra-articular steriods/hyaluronic acid injections and physical therapy are acceptable, but generally less helpful.
- Arthroscopic Debridement: marginal value, generally not recommended. Consider for young, active patients with mild arthritis (Outerbridge I-III). 8% excellent, 72% good, 20% unsatisfactory (Weinstein DM, Arthroscopy 2000;16:471). 87% patient satisfaction (Cameron BD, JSES 2002;11:25).
- Resection arthroplasty: Generally only considered for failed arthroplasty, or infection.
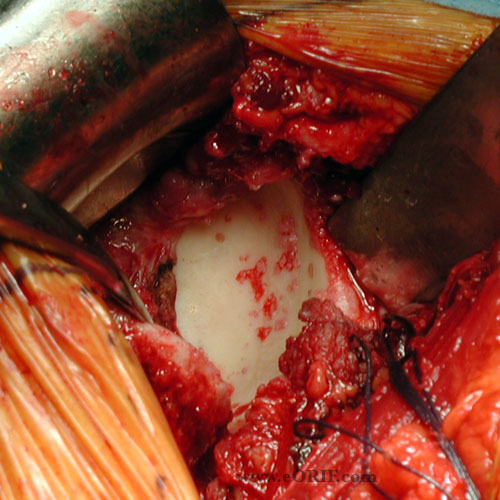
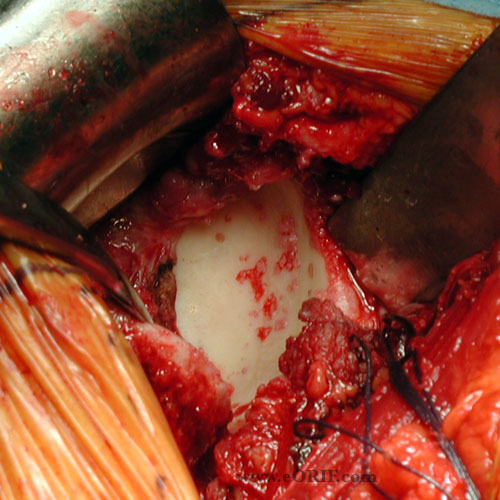
- Interposition arthroplasty: with or without hemiarthroplasty. Graft options: anterior capsule, fascia lata, achilles allograft, lateral meniscal allograft, dura mater, porcine submucosa. 50% excellent, 36% satisfactory, 14% unsatisfactory for biologic glenoid resurfacing with hemiarthroplasty (Kirshnan SG, JBJS 2007;89A:727).
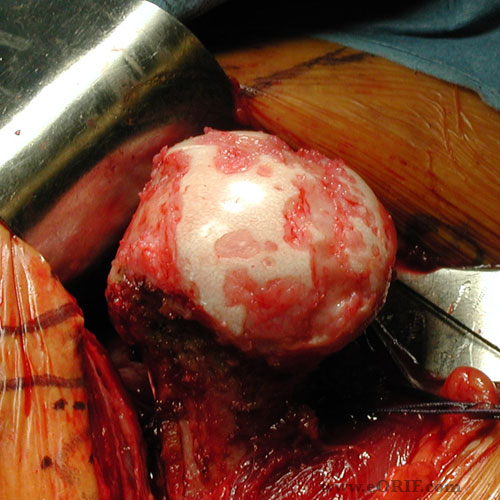
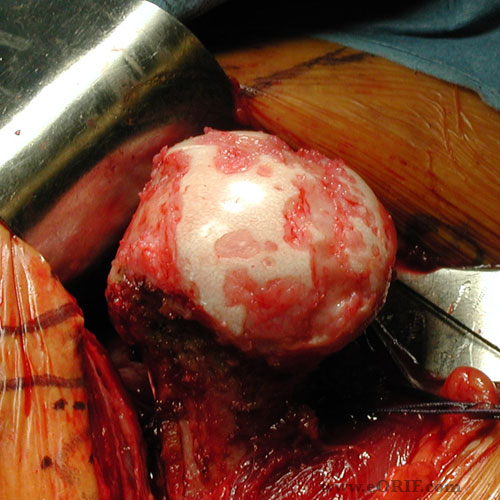
- Hemiarthroplasty: TSA demonstrates improved pain relief, hemiarthroplasty has potential need for revision to TSA. (Gartsman GM, JBJS 2000;82A:26).
- Total shoulder arthroplasty
- Arthrodesis: Generally indicated only if arthritis is associated with muscle paralysis or infection. May be consider in the young heavy laborer who is unwilling to change careers.
Glenohumeral Arthritis Associated Injuries / Differential Diagnosis
- RTC Tear
- Adhesive capsulitis
- Shoulder instability
- AC arthritis
- Calcific tendinitis
- Subacromial impingement
- Fibromyalgia
- Charcot shoulder
- Humeral Head Osteonecrosis
TSA Complications
- Overall 12% incidence (Chin PY, JSES, 2006;15:19) (14%=Cofield RH, ICL 1990;39:449)
- Instability / soft tissue imbalance:
- Rotator cuff tear (Hattrup SJ, JSES, 2006;15:78)
- ectopic ossification
- glenoid loosening
- Peri-Prosthetic fracture (0.5%-3%)
- nerve injury (Lynch NM, JSES 1996;5:53)
- infection: <1% with peri-operative antibiotics
- humeral loosening
- Long-head of biceps rupture
Glenohumeral Arthritis Follow-up Care
Glenohumeral Arthritis Review References
|