|

|
synonyms:
Distal Phalanx Fracture ICD-10
Distal Phalanx Fracture ICD-9
- 816.02(closed),
- 816.12(open)
- multiple sites = 816.03(closed), 816.13(open)
Distal Phalanx Fracture CPT Codes
Distal Phalanx Fracture Etiology / Epidemiology / Natual History
- Common, especially injuries involving the thumb, index and middle fingers.
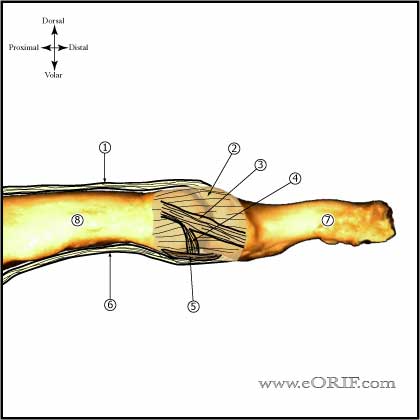
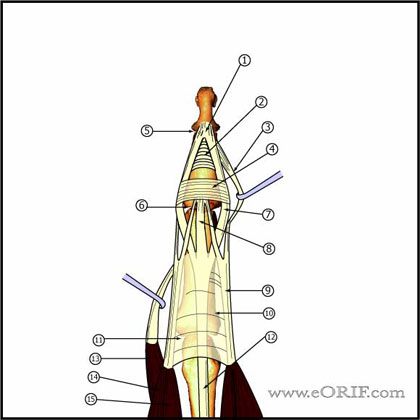
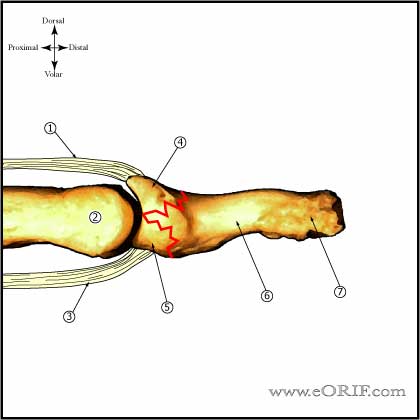
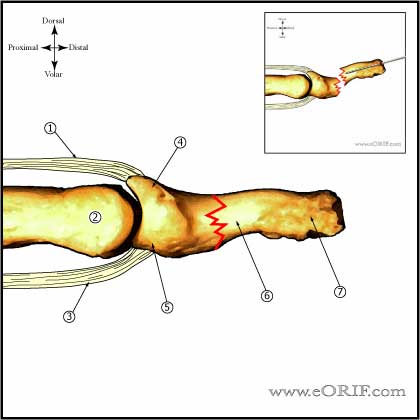
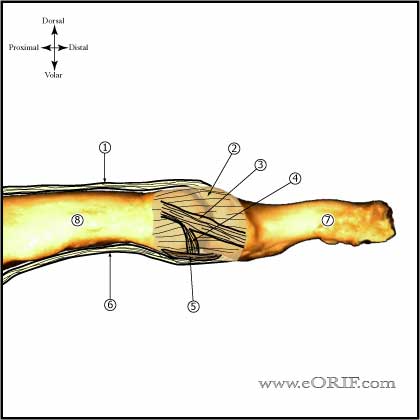
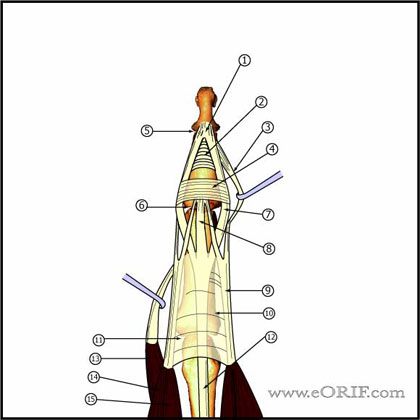
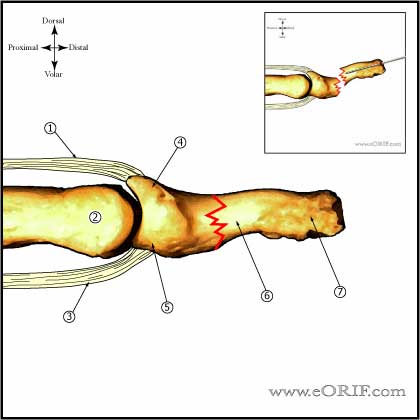
Distal Phalanx Fracture Anatomy
- DIP extension is provided by the the conjoined lateral bands which insert into the base of the distal phalanx
- Conjoined lateral bands are made up of the lateral slips of the extrinsic extensor tendon and the lateral bands from the intrinsic interosseous and lumbrical muscles.
- DIP flexion is provided by FDP insertion into the volar base. Injury to the FDP at this level results in a Jersey Finger.
Distal Phalanx Fracture Clinical Evaluation
- Evaluate finger cascade with flexion. Any overlaps of injured digits indicates need for reduction +/- fixation.
- Subungual hematoma indicates nail bed injury.
Distal Phalanx Fracture Xray
- P/A and lateral views of affected finger.
Distal Phalanx Fracture Classification / Treatment
- Transverse
-Non-displaced: splint (alumifoam or Stack splints) Active ROM at the DIP joint can be allowed since tendon insertions are intact.
-Displaced: CRPP
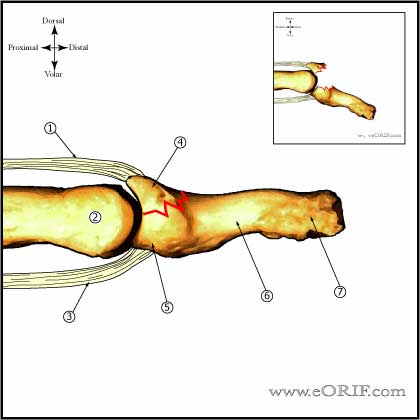
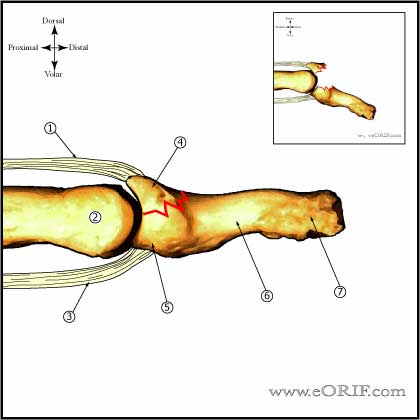
- Dorsal Base
-Can be shearing fractures (usually >20% of articular surface) or avulsion fractures (Mallet finger)
-Non-displaced: splint (alumifoam or Stack splints) with DIP jont immobilized.
-Displaced: Extension block pinning. (Pegoli L, J Hand Surg 2003;28B:15).
-See also Mallet finger.
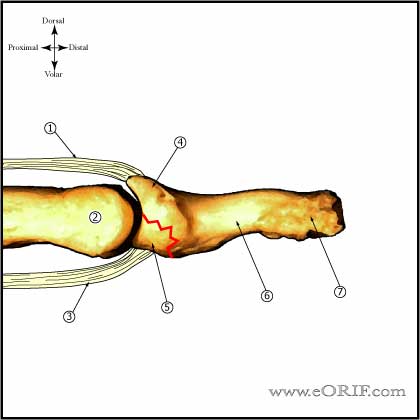
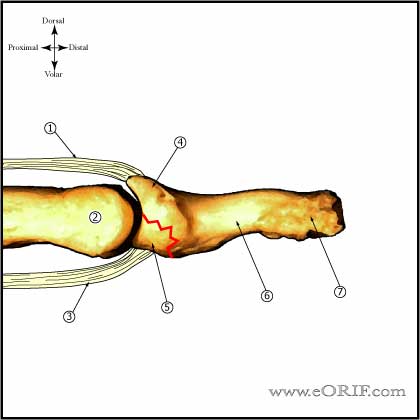
- Volar Base
-Can be shearing fractures (usually >20% of articular surface) or FDP avulsion fractures (Type III Jersey Finger).
-Non-displaced: (rare) splint (alumifoam or Stack splints) with DIP jont immobilized.
-Displaced: ORIF. Large fragment fixation via suture of mini-fragment screws as indicated. See Jersey Finger for technique.
- Tuft Fracture
-Non-displaced: splint (alumifoam or Stack splints)
-Displaced (dorsal surface of the phalanx displaced): CRPP focused on providing a level dorsal surface to support the nail bed.
-Commonly associated with nail bed injurieswhich should be treated concomitantly.
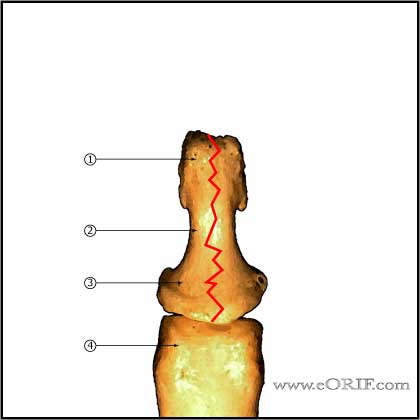
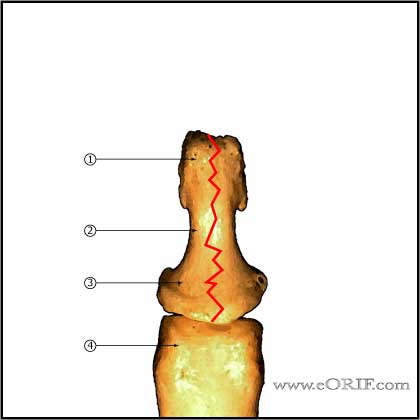
- Longitudinal
-Non-displaced: splint (alumifoam or Stack splints)
-Displaced: CRPP with two transverse 0.028-in or 0.035-in K-wires.
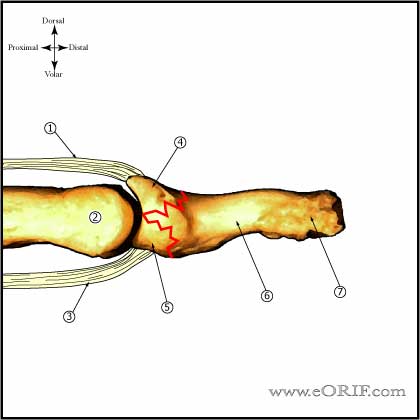
- Pilon
-Non-displaced: rare, tendon forces usually displace fragments. splint (alumifoam or Stack splints)
-Displaced: typically severe injuries. Treatment is dependent on the associated soft-tissue injury. Varying combinations of the techniques desribed for volar base and dorsal base fractures should be employed.
-Often require delayed / secondary DIP joint fusion.
Distal Phalanx Fracture Associated Injuries / Differential Diagnosis
Distal Phalanx Fracture Complications
- Loss of reduction
- Delayed union
- Malunion
- Nonunion
- Tendon adhesion / stiffness
- Nerve or vascular injury
- Hooked nail / nail deformity
Distal Phalanx Fracture Follow-up
- Post-op /Initial: Place in alumifoam extension / clamshell / Stack splint. Elevation.
- 7-10 Days: xray to ensure reduction is maintained. Continued splint, activity modifications. Immobilize as few joints as necessary.
- 6 Weeks: Remove k-wire, wean from splint use as soon as callus is visible on xray. Continue activity modifications. Agressive DIP ROM.
- 3 Months: Resume full activities. Assess ROM.
- 1Yr: assess outcomes / follow-up xrays.
Distal Phalanx Fracture Review References
|