|




|
synonyms: Perthes Disease,
Legg-Calves-Perthes Disease ICD-10
Legg-Calves-Perthes Disease ICD-9
- 732.1 Juvenile osteochondrosis of the hip and pelvis; Leff-Calves-Perthes
Legg-Calves-Perthes Disease Etiology / Epidemiology / Natural History
- disturbance of blood supply to the capital femoral epiphysis
- most common in boys age 3-8
- etiology unknown. Likely related to vascular insult which blocks epiphyseal blood flow in the femoral neck.
- epiphyseal growth retardation, sclerosis, fragmentation and reossification.
- Blood supply is usually reestablished allowing for reossification
- Limited abduction, IR and flexion quite common in severe cases due to femoral head overgrowth and impingement. Secondary acetabular dysplasia can occur. RX: valgus intertrochanteric osteotomy.
- 50% develop OA in adulthood, associated with impingement by aspherical femoral head on the anterolateral acetabular rim and labrum(Mc Andrew JBJS 66A;800, Stubert Iowa study)
- Risk Factors: short stature, delayed bone age, hyperactivity disorder, secondhand smoke, low socioeconomic status.
- impingement form deformed femoral heads can lead to acetabular labral tears associated with intermittent sharp groin pain, locking and clicking. Labral tears diagnosed with contrast MRI. Treatment is open or scope debridement.
- Prognosis depends on age at diagnosis, and amount of head involvement
- outcome correlates with sphericity of femoral head
Legg-Calves-Perthes Disease Anatomy
Legg-Calves-Perthes Disease Clinical Evaluation
- Painless limp with Trendelberg gait.
- Hip/groin pain
- Decreased IR, decreased Abduction
Legg-Calves-Perthes Disease Xray / Diagnositc Tests
- AP and lateral pelvis films, lateral can be frog-legged or cross table
- characteristic sequence of changes from epiphyseal growth retardation, sclerosis, fragmentation to reossification. Leads to variable coxa magna and deformation
- 20% bilateral, rarely symmetrical
- If symmetrical consider epiphyseal dyplasia and hypothyroidism
- Labs: CBC, ESR, CRP consider to eval for infection in DDX.
Legg-Calves-Perthes Disease Classification / Treatment
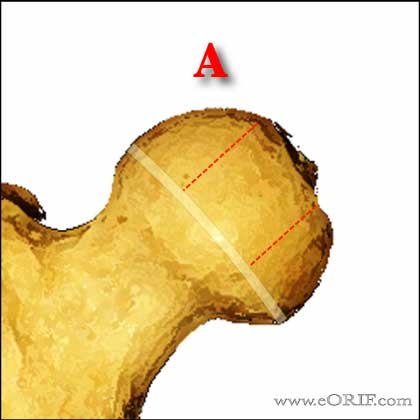
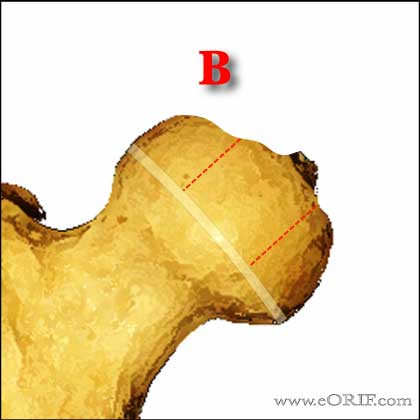
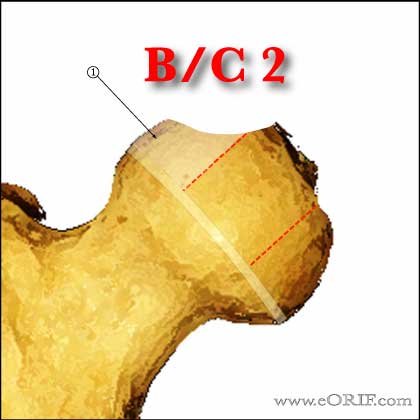
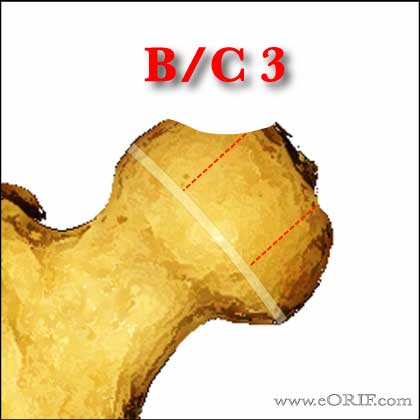
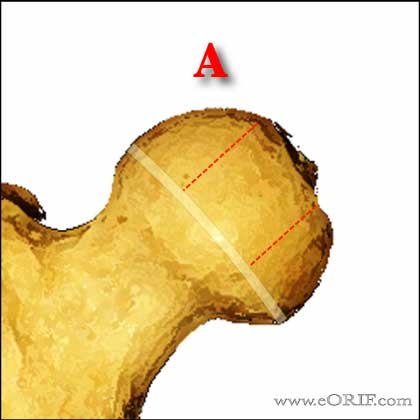
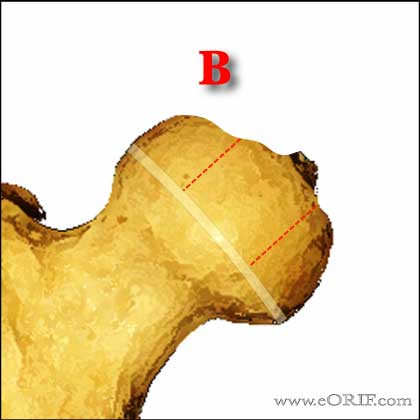
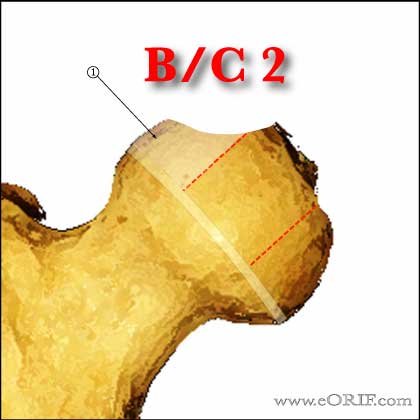
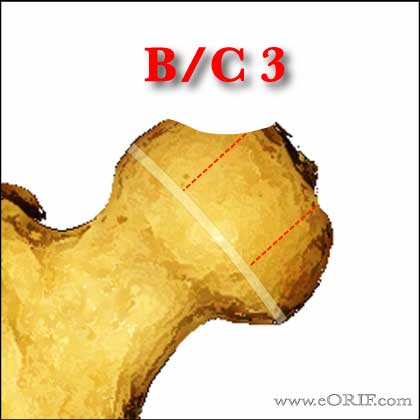
- Lateral pillar classification; determined on the AP xray. Lateral pillar-lateral 25% of the head; central pillar=cetral 50%; medial pillar=medial 25%. (Herring JA, JBJS 2004;86A:2103).
- Group A=no involvement of lateral pillar
-Treatment Age < 8y/o: NSAIDs, ROM exercises, good outcomes regardless of treatment
-Treatment Age >8y/o: NSAIDs, ROM exercises
- Group B=>50% of lateral pillar height maintained
-B/C 1=lateral pillar >50% height, but 2-3mm width
-B/C 2 = lateral pillar >50% height, but little ossification
-B/C 3 = lateral pillar 50% height, but depressed relative to central column.
-Treatment Age < 8y/o: NSAIDs, ROM exercises, good outcomes regardless of treatment.
-Treatment Age >8y/o: femoral and/or rotational pelvic osteotomy. Gaol: keep femoral head contained within acetabulum. May require presurgical traction, bracing or physical therapy.
- Group C=<50% of lateral pillar height maintained
-Treatment Age < 8y/o: poor outcome regardless of treatment.
-Treatment Age >8y/o: poor outcome regardless of treatment.
- Catteral Classification (Catterall A, Acto Orthip Belg 1980;46:346).
Perthes Treatment
- goals=maintain physiologic ROM, particularly abduction and physical contact. Goal is a spherical congruent joint.
- options=nothing, intermittent traction, abduction orthosis(Meehan, JBJS 74A 11992 showed bracing, and physcial therapy not helpful), surgery
- activity limitation, PT, abduction splinting or casting. Containment bracing has not been shown to be useful.
- Age >6: prognosis is good. Generally treated with ROM exercises to prevent contracture (Herring JA, JBJS 2004;86:2121).
- surgery=innominate osteotomy, shelf arthroplasty, intertrochanteric varus osteotomy, valgus osteotomy
- Weiver JPO 11;20 1991=varus osteotomy
- Sponsellar JBJS 1988 70A;1131=pelvic/femur osteotomy
- Shelf Acetabuloplasty indicated in patients in the healed phase with residual head deformity and pain (adolescents). (Daly K, JBJS 1999;81Br:380).
- Ibandronate has been shown to prevent femoral head deformity in a pig model (Kim H, JBJS 2005;87A;550)
Legg-Calves-Perthes Disease Associated Injuries / Differential Diagnosis
- Hypothyroidism
- Gaucher’s Disease
- Hemophilia
- Sickle Cell
- Myers Dysplasia
- SED
- MED
- toxic synovitis,
- Septic arthritis
- Osteomyelitis
- JRA
- TB
Legg-Calves-Perthes Disease Complications
- Chronic Pain
- Arthritis
- Loss of motion
Legg-Calves-Perthes Disease Follow-up Care
Legg-Calves-Perthes Disease Review References
- Clancy M, Steel HH: the effect of an incomplete intertrochanteric osteotomy on LCP disease. JBJS 19985;67:213-216.
- Salter RB, Thompson GH: LCP disease: the prognostic significance of the subchondral fracture and a two-group classification of the femoral head involvement. JBJS 1984;66:479-489.
- DeSanctis N, Rega Anm Rondinella F: Prognostic eval of LCP disease by MRI: Part I. The role of physeal involement. JPO 2000;20:455-462.
- Pathomorphogenesis and new classification. JPO 2000;20:463-470.
- Ibrahim T, Little DG. The Pathogenesis and Treatment of Legg-Calvé-Perthes Disease. JBJS Rev. 2016 Jul 19;4(7). pii: 01874474-201607000-00003. doi: 10.2106/JBJS.RVW.15.00063. PubMed
- Lovell and Winter's Pediatric Orthopaedics 2012

°
|