|
|
synonyms:Concussion, closed head injury, traumatic brain injury
Concussion ICD-10
- S06.0X0A Concussion without loss of consciousness, initial encounter
- S06.0X0D Concussion without loss of consciousness, subsequent encounter
- S06.0X0S Concussion without loss of consciousness, sequela
- S06.0X1A Concussion with loss of consciousness of 30 minutes or less, initial encounter
- S06.0X1D Concussion with loss of consciousness of 30 minutes or less, subsequent encounter
- S06.0X1S Concussion with loss of consciousness of 30 minutes or less, sequela
- S06.0X9A Concussion with loss of consciousness of unspecified duration, initial encounter
- S06.0X9D Concussion with loss of consciousness of unspecified duration, subsequent encounter
- S06.0X9S Concussion with loss of consciousness of unspecified duration, sequela
- S14.0XXA Concussion and edema of cervical spinal cord, initial encounter
- S14.0XXD Concussion and edema of cervical spinal cord, subsequent encounter
- S14.0XXS Concussion and edema of cervical spinal cord, sequela
- S24.0XXA Concussion and edema of thoracic spinal cord, initial encounter
- S24.0XXD Concussion and edema of thoracic spinal cord, subsequent encounter
- S24.0XXS Concussion and edema of thoracic spinal cord, sequela
- S34.01XA Concussion and edema of lumbar spinal cord, initial encounter
- S34.01XD Concussion and edema of lumbar spinal cord, subsequent encounter
- S34.01XS Concussion and edema of lumbar spinal cord, sequela
- S34.02XA Concussion and edema of sacral spinal cord, initial encounter
- S34.02XD Concussion and edema of sacral spinal cord, subsequent encounter
- S34.02XS Concussion and edema of sacral spinal cord, sequela
- See all concussion ICD-10 codes.
A- initial encounter
D- subsequent encounter
S- sequela
Concussion ICD-9
- 850 Concussion, includes commotio cerebri
- 850.0 With no loss of consciousness
- 850.9 Concussion, unspecified
- 959.01 Head injury, unspecified. Excludes concussion
Concussion Etiology / Epidemiology / Natural History
- Conconssion = complex pathophysiologic process affecting the brain that is induced by traumatic biomechanical forces.
- Head injury causes increased need for glycolysis and decreased cerebral blood flow which places the brain at increased risk for subsequent injury.
- More common in competition than during practice.
- Football (47%), girls’ soccer (8%), and boys’ wrestling (6%). (OKU-11)
- Football players: linemen have highest incidence, followed by tight ends, running backs, and linebackers (OKU-11).
Concussion Anatomy
Concussion Clinical Evaluation
- Confusion, altered mental status after collision in contact sports, direct blow from ball etc (baseball, lacrosse, hockey).
- Short term retrograde amnesia, LOC, disorientation, delayed verbal/motor response, headache, nausea/vomiting, visual disturbance, emotional liability, dizziness, speech disturbance, drowsiness, disequilibrium.
- Associated with: football, hockey, soccer, lacrosse, field hockey, softball, baseball.
- Evaluate for palpable calvariul malalignment, cranial nerve injury, rhinorrhea, otorrhea, raccoon eyes, Battle's sign, hemotympanum which indicated associated skull fracture.
- Determine orientation: Score of the game? Name of the opponent? Color of opponents jersey? Team record? Current quater in game? Person/Place/Time.
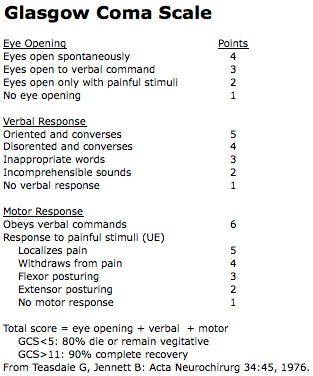
- Neuro Exam: pupillary response, cranial nerve function, UE/LE strength/sensation, cerebellar tasks, gait.
- Standardized Assessment of Concussion (SAC) (McCrae M, J Athletic Training 2001;36:274)
Concussion Xray / Diagnositc Tests
Concussion Classification / Treatment
- SCAT3 assessment
- All concusions must be evaluated by a physician. Patients with LOC, neuro deficit, significant amnesia, nausea/vomiting, evidence of skull fracture should be evaluated with CT. Patients with normal CT scans can generally be discharged as long as adequate observation by responsible caregiver is available.
- ISCS-Vienna Conference classification: Simple; Complex
- Simple: injury that progressively resolves over 7-10 days. Treatment: rest until all symptoms resolved, graded exertion before return to sport.
- Complex: persistent symptoms, or specific sequelae or prolonged loss of consciousness, or prolonged cognitive impairment, or mutliple concussions. Treatment should be with a multi-disciplinary approach.
- Return to play: players should not be allowed to return to play in current game/practice. Players must be regularly monitoried for first 2-3 hours after concussion and not left alone. Return to play is only allowed after graded exertion without symptoms. Any symptoms precludes return to play.
- Graded exertion: rest > light aerobic exercise > sport specific exercise > non-contact training drills > full contact training after medical clearance > Game play. If any symptoms occur the patient should drop back to previous asymptomatic level and progress again after 24 hours.
- Old grading systems and recommendations may be obsolete
- Grade 1: Patients must be symptom free with mild to moderate exertion (cardiovascular challenge) before return to play.
- Grade 2: loss of consciousness. 4-week period out of sport. May return to sport after 4 weeks if the patient is completely symptom free from for the last week prior to return.
Concussion Associated Injuries / Differential Diagnosis
- Second Impact Syndrome (SSI): occurs when return to sport is allowed prior to complete resolution of symptoms. Second head injury leads to rapidly progressing deterioration which can involve the brainstem and lead to sudden death. (Cantu RC, Cin Sports Med 1998;17:37).
- Subdural hematoma: disruption of the venous blood supply. LOC, focal neurolgic deficit, slow deterioration in mental status. Simple subdural hematoma = no underlying cerebral edema/contusion; 20% mortality. Complex subdural hematoma = with cerebral edema/contusion; 50% mortality.
- Epidural hematoma: disruption of the meningeal arterial vasculature; middle meningeal artery=most common. Initial LOC followed by recovery/lucid interval with later development of headache, mental status deterioration, ipsilateral pupil dilation, LOC, decerebrate posturing with weakness on the opposite side of the bleed.
- Subarachnoid hemorrhage (rare)
- Cerebral contusions: damaged parenchymal vessels on surface of the brain. More commonly on the inferior surfaces of the frontal and temporal lobes due to bony ridges in skull. Brief LOC, prolonged posttraumatic confusion may have increased ICP or focal neurologic deficits.
- Intracerebral hemorrhage: bleeding in the small arterioles within the brain parenchyma; generally frontal or temporal lobes. Headaches, confusion, nausea, vomiting, focal neuro deficit, LOC.
- Scalp lceration
- Skull fracture
- Cervical spine injury
Concussion Complications
- Seizures: generally within 1 week from injury.
- Post-concussive syndrome: persistent headache, inability to concentrate, irritability, fatigue, vertigo, sleep and gait disturbances, visual complaints, emotional liability.
- Second Impact Syndrome
- Chronic traumatic encephalopathy: dementia pugilistica, 9-25% of professional boxers.
Concussion Follow-up Care
- Effects of concussions may be cumulative. Athletes with >3 concussions are much more likely to sustain a recurrent concussion and should consider avoiding contact sports.
- TBI Rehab (NIH Consens Statement 1998;16:1)
Concussion Review References
- Wojtys EM, AJSM, 1999;27:676 (contains AOSSM guidelines)
- McCoy P, Br J Sports Med 2005;39:196. (contains international guidelines)
- Kelly JP, Neurology 1997;48:581
- Cantu RC, Clin Sports Med 1998;17:45
- Guskiewicz KM, JAMA 2003;290:2549
- National Center for Injury Prevention and Contral: Traumatic Brain Injury in the US: A report to congress.
- Putukian M. The acute symptoms of sport-related concussion: Diagnosis and on-field management. Clin Sports Med. 2011 Jan;30(1):49-61
- McCrory P, Meeuwisse W, Johnston K, Dvorak J, Aubry M, Molloy M, Cantu R. Consensus statement on concussion in sport - the Third International Conference on Concussion in Sport held in Zurich, November 2008. Phys Sportsmed. 2009 Jun;37(2):141-59.
- d'Hemecourt P. Subacute symptoms of sports-related concussion: outpatient management and return to play. Clin Sports Med. 2011 Jan;30(1):63-72,
- Aubry M, Clin J Sport Med 2002;12:6)
- °
|