|

|
synonyms:
Compartment Syndrome ICD-10
- T79.A0XA - Compartment syndrome, unspecified, initial encounter
- T79.A11A - Traumatic compartment syndrome of right upper extremity, initial encounter
- T79.A12A - Traumatic compartment syndrome of left upper extremity, initial encounter
- T79.A19A - Traumatic compartment syndrome of unspecified upper extremity, initial encounter
- T79.A21A - Traumatic compartment syndrome of right lower extremity, initial encounter
- T79.A22A - Traumatic compartment syndrome of left lower extremity, initial encounter
- T79.A29A - Traumatic compartment syndrome of unspecified lower extremity, initial encounter
- T79.A3XA - Traumatic compartment syndrome of abdomen, initial encounter
- T79.A9XA - Traumatic compartment syndrome of other sites, initial encounter
- see all Compartment Syndrome ICD-10
A- initial encounter
D- subsequent encounter
S- sequela
Compartment Syndrome ICD-9
- 958.90 Compartment syndrome, unspecified
- 958.91 Traumatic compartment syndrome of upper extremity Traumatic compartment syndrome of shoulder, arm, forearm, wrist, hand, and fingers
- 958.92 Traumatic compartment syndrome of lower extremity Traumatic compartment syndrome of hip, buttock, thigh, leg, foot, and toes
Compartment Syndrome Etiology / Epidemiology / Natural History
- Elevated interstitial pressures lead to prolonged ischemia which causes irreversible destruction of myoneural tissue and subsequent fibrosis.
- Etiology: Closed/Open Fracture, Exertional states, GSW, IV/A-lines, Hemophiliac/coagulopathy, Intraosseous IV(infant), Snake bites, Blunt trauma, vascular occlusion, Cast/dressing Burns/electrical
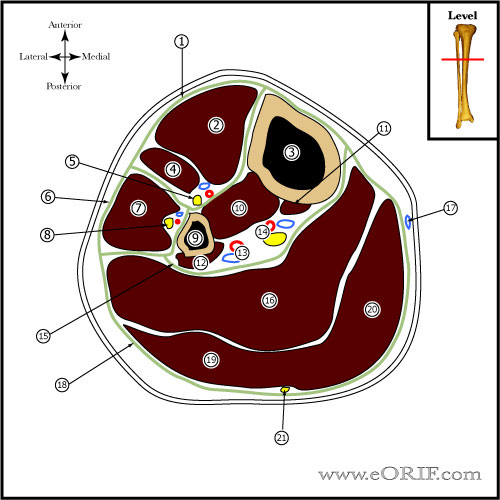
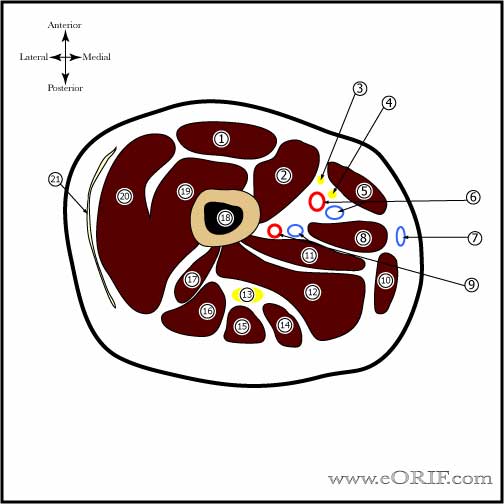
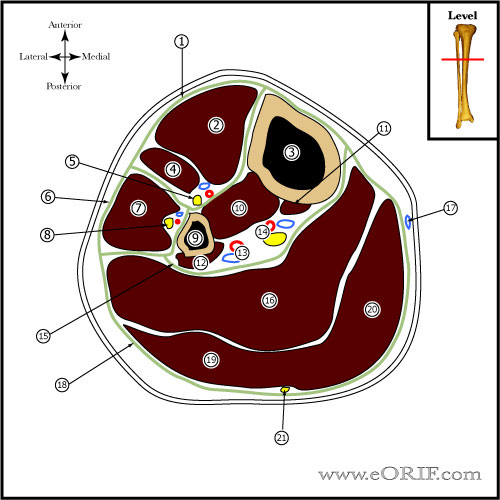
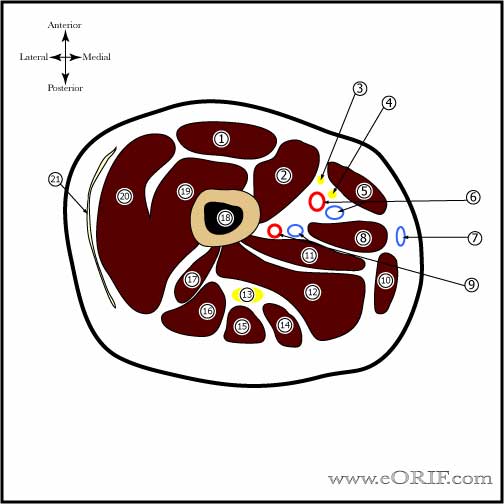
Compartment Syndrome Anatomy
- Arm Compartments: (1) Anterior, (2)Posterior
- Forearm Compartments: (1)Dorsal (extensors) (2)Volar (flexors) (3)Mobile wad(Brachioradialis, ECRL, ECRB)
- Hand Compartments:
- Thigh Compartments:
- Leg Compartments: (1) Anterior, (2) Lateral, (3)Superficial Posterior, (4)Deep Posterior.
- Foot Compartments: considered to have 4 or 9 compartments.
- (1)medial; abductor hallucis and flexor hallucis brevis; bounded by plantar aponeurosis, intermuscular septum and by 1st metatarsal. Pressure measurement: base of 1st MT advanced @2cm into the abductor hallucis
- (2) Lateral; abductor digitia mini, flexor digitorum brevis-5th, opponens-5th; bounded by 5th metatarsal, plantar aponeuorosis, intermuscular septum. Pressure measurement: 5th MT shaft advance needle 1cm medially and plantarly.
- (3)Central; flexor difitorum brevis, lumbricals, quadratus plantae, adductor hallucis; bounded by plantar aponeurosis, intermuscular septum, osseofascial tarsometatarsal structrues. Pressure measurement: base of 1st MT directing needle lateral and plantar through the abductor hallucis.
- (4)Interosseous; 7 interosseous muscles; bounded by interosseus fascia and metatarsals. Pressure measurement: 2nd, 3rd, 4th webspaces advanced plantarly @2cm past extensor fascia.
- Calcaneal compartment;quadratus plantae, laterl plater nerve. Communicates with the deep posterior compartment of the leg and the central compartment of the foot. Pressure measurement: 5cm distal and 2cm inferior to medial malleolus directed toward posterior calcaneal tuberosity
- Associated with up to 17% of calcaneous fractures.
Compartment Syndrome Clinical Evaluation
- Five "P"'s=pain, paralysis, pulselessness, paresthesias, pallor. If all five signs are present, particularily pulselessness, the process is probably irreversible.
- Pain, often severe, unremitting, non-responsive to analgesics, is the most sensitive and earliest indicator.
- Pain with passive stretching of muscles in the compartment in question is the key finding in diagnosing compartment syndrome.
- Document sensory deficit, motor deficit, pulses and diastolic blood pressure.
- Indications for compartment release remain controversial. (Prayson MJ, J Trauma, 2006;60:1037).
- in an unconscious patient measurement of compartment pressures may be the only reliable indicator of compartment syndrome
Compartment Syndrome Xray / Diagnositc Tests
- Xrays of the affected extremity should be taken to evaluate for associated injuries / fractures.
- Intracompartmental pressure measurements: Stryker monitor or arterial line connected to 18 gauge needle. Side-port needles or slit catheters are more accurate then straight needles. History method = Infusion Technique (Whitesides CORR 1975),
- Measurement should be taken within 5cm of zone of injury (Heckman MM, JBJS 1994;76:1285).
- Fasciotomy indicated if compartment pressure is within 30mmHg of the diastolic blood pressure. (McQueen MM, JBJS 1996;78B:99-104).
Compartment Syndrome Classification / Treatment
- Treatment = fasciotomy of the affected compartment.
- Indications for prophylactic fasciotomy: >6hours of limb ischemia high energy injury, blast injury; if any concerns for subsequent compartment syndrome, do the fasciotomy.
- Arm- posterior and anterior compartments. Volar(Henry) incisions from forearm can be extended up into an anterolateral incision in arm to release both compartments.Try to leave large medial skin flap over antecubital fossa to cover NV structures.
- Forearm=dorsal, volar, mobile wad.
- Hand- 10 compartments: 4 dorsal interossei, 3 volar interossei, thenar, hypthenar, adductor pollicis
- Thigh-- Three compartments (Anterior (quadriceps), Medial (adductor; rarely released, Posterior (hamstrings)) (Schwartz JT Jr, JBJS 1989;71A:392-400.)
- Leg- anterior, lateral and deep&superficial posterior. CPT: 27602(anterior and/or lateral and posterior compartments), 27600(fasciotomy leg anterior/lateral compartments only), 27601(posterior compartments only). For fasciotomy with debridement see 27892-27894)
- Foot - 5 compartments: Interosseous, lateral, central, medial, calcaneal. (Manoli J Orthop Trauma 6:223;1992). Two dorsal incisions overlying the 2nd and 4th MT, bluntly dissected into the web spaces for decompression. Medial incision along the inferior border of the 1st MT, superior to the abductor. Expose the abductor by incising the superior fascia and enter central compartment with further lateral dissection. Calcaneal
Compartment Syndrome Associated Injuries / Differential Diagnosis
- Tibia fractures (open and closed)
- Ipsilateral tibia and femur fracture
- Distal humerus fractures
- Forearm fractures (GSW)
- Vascular injury
- Muscle Contusion
- Shin-splints
- Coagulopathy
- Shock
- Ischemia
- DVT
Compartment Syndrome Complications
- Myonecrosis
- ischemic contractures
- chronic pain
- limb paralysis / nerve palsy
- dry gangrene
- Amputation
- Incisional scar
Compartment Syndrome Follow-up Care
- Repeat I&D's until sofot tissue environment improves
- Delayed primarily closure vs skin grafting when soft tissues permit.
Compartment Syndrome Review References
- Burris DC, Emergency War Surgery, 3rd ed. 2004
- Tornetta P III, Templeman D: Compartment syndrome associated with tibial fracture. Instr Course Lect 1997;46:303-308.
- Elliott KG, JBJS 2003;85Br:625)
- Heckman MM. JBJS 1994 76A;1285-1292
|