|
|
Fracture Fixation Criteria (requirements prior to fixation) (Tscherne H, CORR 1998;347:62).
- No evidence of increaseing infiltration on CXR
- Balanced or negative fluid balance
- PaO2/FIO2 >250mmHg within previous 24hrs
- Pulmonary artery pressure <35mmHg
- Peak inspiratory pressure <35 cm H20
- Platelet count >95,000/mm3
- Leukocyte count >2,000/mm3 and <12,000/mm3. No signs of sepsis
- Intracranial pressure 15cm H20.
- Stable CT of the head with no signs of increasing hygroma
Indications to minimize / delay fracture fixation
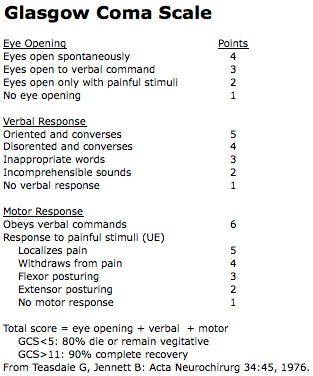
- Severe head injury GCS <8
- Severe thoracic/lung contusion with continuous intrabronchial bleeding of edema formation
- MI
- Clotting disorder
- Hypothermia (<32º).
ABC's
- A: Airway and c-spine protection
- B: Breathing and ventilation
- C: Circulation / hemorrhage control
- D: Disability / neurologic status
- E: Exposure / environment
Primary Survey
- Vitals(blood pressure, O2 sat, heart rate, respiratory rate)
- 2 large bore peripheral IVs
- AP chest, AP pelvis, lateral C-spine
- Consider NG tube, urinary catheter, EKG
- Avoid: hypothermia, acidosis and coagulopathy
Hemorrhagic Shock
- IV fluid bolus 2L for adults, 20mL/kg for children.
- Control hemorrhage, tourniquet if necessary. If no source is identified FAST or CT indicated.
- If responce to fluid bolus is weak severe blood loss is present (>40%): Consider blood transfusion.
- If responce to fluid bolus is transient, moderate blood loss is present (20-40%): Consider blood transfusion.
- If vitals normalize blood loss is minimal.
Tension Pneumothorax
- CE: shortness of breath and dyspnea
- PE: tachypnea, tachycardia, trachea shifted to the right, decreased breath sounds in the affected lung, subcutaneous emphysema.
- RX: large gauge needle placement into the second intercostal space in the midclavicular line / ER or OR chest tube placement.
ARDS (Adult Respiratory Distress Syndrome)
- Diffuse bilateral infiltrates on CXR
- Refractory hypoxemia (PaO2/FiO2 <200mmHg regardless of PEEP level)
- No evidence of left heart-failure; wedge pressure < 18mmHg
- Predisposing condition / acute onset
Markers of Immune Reactivity
- Interleukin-6
- Human leukocyte antigen-DR class II
Injury Severity Score, (ISS)
- an anatomical scoring system that provides an overall score for patients with multiple injuries.
- Each injury is assigned an Abbreviated Injury Scale (AIS) score from 1-5 and is allocated to one of six body regions (Head, Face, Chest, Abdomen, Extremities (including Pelvis), External). Only the highest AIS score in each body region is used.
- 3 most severely injured body regions have their score squared and added together to produce the ISS score
- ISS scores = 0 to 75.
- If an injury is assigned an AIS of 6 (unsurvivable injury), the ISS score is automatically assigned to 75.
- ISS >16 =10% mortality
- ISS <30 –good prognosis unless associated with severe head injury
- ISS >60 usually fatal
- ISS virtually the only anatomical scoring system in use and correlates linearly with mortality, morbidity, hospital stay and other measures of severity.
- It's weaknesses are that any error in AIS scoring increases the ISS error, many different injury patterns can yield the same ISS score and injuries to different body regions are not weighted. Also, as a full description of patient injuries is not known prior to full investigation & operation, the ISS (along with other anatomical scoring systems) is not useful as a triage tool.
- Baker SP et al, "The Injury Severity Score: a method for describing patients with multiple injuries and evaluating emergency care", J Trauma 14:187-196;1974
- Copeland, CE AR:Mortality in patients with bilateral femoral fractures. J Orthop Trauma 1998:12 :315-319.
Multitrauma
- ARDS: increased risk with femoral fracture, combined abdomen and extremity injuries
- Fracture fixation within 2 days of injury is associated with an increased inflammatory response as compared to delayed fixation (5-8days) in multitrauma patients. Increased inflammation may lead to increased risk of ARDS, DIC, end organ damage.
- Consider temporary external fixation especially for femur fractures in multitrauma patients. (Pape HC, J Trauma 2002;53:452).
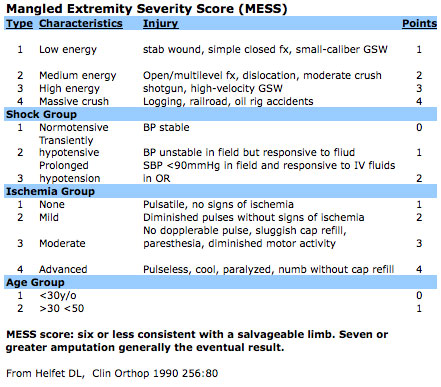
Limb Salvage
- Absent plantar sensation is not an indication for primary amputation and is not prognostic for long-term plantar sensory status or functional outcome. (Bosse MJ, J Bone Joint Surg Am. 2005 Dec;87(12):2601-8. MacKenzie EJ, JAAOS 2006;14(10 Spec No.):S205-10.)
References
- Sears BW, JAAOS 2009;17:255
- Pape HC, Hildebrand F, Pertschy S, Zelle B, Garapati R, Grimme K, Krettek C, Reed RL 2nd. Changes in the management of femoral shaft fractures in polytrauma patients: from early total care to damage control orthopedic surgery. J Trauma. 2002 Sep;53(3):452-61
- Pape HC, Grimme K, Van Griensven M, Sott AH, Giannoudis P, Morley J, Roise O, Ellingsen E, Hildebrand F, Wiese B, Krettek C. EPOFF Study Group. Impact of intramedullary instrumentation versus damage control for femoral fractures on immunoinflammatory parameters: prospective randomized analysis by the EPOFF Study Group. J Trauma. 2003 Jul;55(1):7-13.
- Pape HC, Rixen D, Morley J, Husebye EE, Mueller M, Dumont C, Gruner A, Oestern HJ, Bayeff-Filoff M, Garving C, Pardini D, van Griensven M, Krettek C, Giannoudis P. EPOFF Study Group. Impact of the method of initial stabilization for femoral shaft fractures in patients with multiple injuries at risk for complications (borderline patients). Ann Surg. 2007 Sep;246(3):491-9
|