|



|
synonyms: total knee replacement, TKA, artificial knee, total knee arthroplasty
TKA CPT
Knee Arthroplasty Applicable ICD-10 Codes
- M17.0 - Bilateral primary osteoarthritis of knee
- M17.10 - Unilateral primary osteoarthritis, unspecified knee
- M17.11 - Unilateral primary osteoarthritis, right knee
- M17.12 - Unilateral primary osteoarthritis, left knee
- Z47.33 - Aftercare following explantation of knee joint prosthesis
- Z96.651 - Presence of right artificial knee joint
- Z96.652 - Presence of left artificial knee joint
- Z96.653 - Presence of artificial knee joint, bilateral
- Z47.33 - Aftercare following explantation of knee joint prosthesis
TKA Anatomy
- Knee Anatomy
- Medial plateau is larger and concave, lateral plateau is smaller and convex
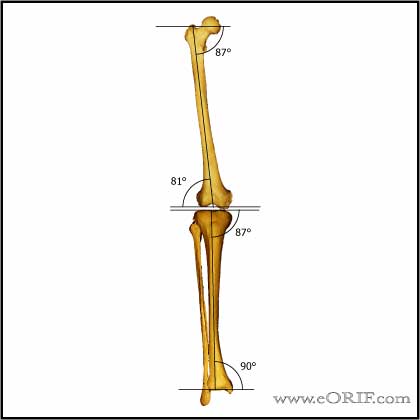
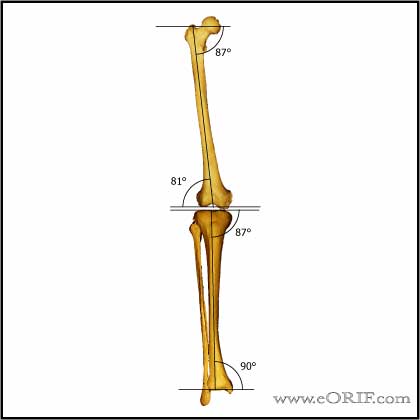
- Mechanical axis=line drawn from center of femoral head to center of ankle joint, should pass through center of knee.
- Epicondylar axis is @3 degrees externally rotated as compared to posterior condylar line
- Distal femoral condyles are in 9 valgus relative to femoral anatomic axis
- Tibial plateau is in 3 varus relative to tibial axis
- Anatomic axis=line drawn down center of tibial or femur.
- Tibiofemoral angle=angle between tibial and femoral anatomic axis=6
- Tibial plateau has @10 posterior slope
- 3 compartments =medial, lateral, patellofemoral
- Rollback = the posterior movement of the tibiofemoral contact point the occurs with knee motion from extension to flexion.
- Paradoxical rollback = tibiofemoral contact point moves anteriorly with knee motion from extensino to flexion. Paradoxical rollback occurs in the anterior cruciate-deficient, posterior cruciate-retaining total knee prosthesis.
- During knee flexion, the tibia internally rotates for the first 20 degree, then maintains this rotational position until flexion past 90 degrees when internal rotation increases. (Coughlin KM, J Arthroplasty 2003;18(8):1048-1055).
TKA Indications
- Disabling knee pain due to severe arthritis which has failed non-operative management.
- Severe patellofemoral arthritis.
- Ideal pt is thin, old, sedentary, flexion contracture>10, ROM >90.
TKA Contraindications
- Patients with lymphedema, diabetes and arrhymia requiring anticoagulation are at higher risk of developing periprosthetic joint infection.
- Infection
- Nonfunctioning knee extensors
- Neuropathic joint
- Neuromuscular dysfunction
- Severe vascular disease
- Relative:young age, active, obesity
- independent predictors for periprosthetic joint infection: higher American Society of Anesthesiologists score, morbid obesity, bilateral arthroplasty, knee arthroplasty, allogenic transfusion, postoperative atrial fibrillation, myocardial infarction, urinary tract infection, and longer hospitalization. (Pulido L, CORR 2008;466:1710)
TKA Alternatives
- Arthroscopic debridement-indicated for pt with ,1yr symptoms, nl alignment, mechanical symptoms.
- Unicompartmental knee- indications flexion cont <15, ROM >90, age >60, sedentary: rehab easier, costs less, quicker ROM, preserves ligamants/proprioception, 92% last 10yr, 15yrs = 60% working. Creates bone defect which often must be filed with allograft
- High tibial osteotomy-for varus deformity <15, young pt, vigorous lifestyle, isolated medial arthritis, obese, ROM>90, flexion contracture<15. Need full length weight bearing radiographs. comps=under/overcorrection, AVN, patella baja, peroneal N. injuries, anterior compartment syndrome. Lasts 7-10 yrs. Osteotomy contraindicated in inflammatory arthropathy.
- Distal femoral osteotomy-for valgus deformity <15, indications as above
- Arthodesis-indicated for infection, failed TKA, young active patients, soft tissue defects, absent extensor mechanism, neuropathic joint disease. fusion in 10-15 flexion and 0-7 valgus. complications=infection, non/malunion, pain.successful in 80-90% of failed condylar components, 55% of failed hinged prosthesis.
TKA Pre-op Planning / Special Considerations
- Maximize Patient pre-opL. Hgb>12.0, HgbA1C<8, BMI<40, No smoking, albumin >3.0 g/dl. Consider Vitamin D.
- Adequate muscle relaxation, discuss with anesthesia. Thigh tourniquet with knee flexed to maximize amount of quad below tourniquet.
- Incision: usually anterior midline skin c medial parapatellar capsulotomy. Consider lateral parapatellar for >15 valgus knees.
- Tibial:tibial cut=perpendicular to tibial mechanical axis. Tibial mechanical and anatomic axis usually equal. For PCL retaining TKA posterior slope = 6°-9°. For PCL sacrificing TKA posterior slope = 0°-3°.
- Patella: Restore original patellar thickness after resurfacing. Normal patella thickness=23-25mm. Minimum of 15mm postresection required to avoid patellar fracture.
- Gaps:
- Extension gap normal, Flexion gap tight: downsize the femoral component or add posterior slope to the tibia resection; in posterior cruciate-retaining TKA consider recession or release of the posterior cruciate ligament to loosen the flexion gap.
- Flexing the femoral component tightens the flexion gap.
- Extension tight, flexion tight: Decrease the tibial component thickness or resect more tibia
- Resecting more distal femur only loosens the extension gap.
- Femur: femur cut angle=valgus cut angle-usually 5-7°=angle between femoral anatomic and mechanical axis=femoral cut should be perpendicular to mechanical axis. Tall valgus cut=5, Short valgus cut=7
- Femoral Rotation: parallel to the epicondylar axis of the femur. Epicondylar axis is externally rotated 3°-5° relative to the posterior condylar axis. AP axis of the femur (Whiteside's line) is perpendicular to the epicondylar axis. Beware of hypoplastic lateral femoral condyle causing erroneous Internal rotation when posterior referencing valgus knees.
- Balancing: if gap is Symmetric adjust tibia, if asymmetric adjust femur.
- Landmarks: Joint line should be @1.5cm above the tip of the fibular head. Also consider measuring the distance from the adductor tubercle to the joint line on the unaffected side for comparision.
- Patellofemoral articulation-avoid IR femoral component(landmarks=A/P axis of femur, epicondylar axis which is in slight ER, posterior condylar axis. Avoid IR tibia. Medialize/centralize patellar component.
- Polyethylene thickness must be at least 8mm to keep contact stresses below the yield strength of UHMWPE.
- If between sizes using posterior reference use larger size to avoid notching
- If between sizes using anterior referencing use smaller size
- Femoral Notching: Notching decreases femoral bending strength by 18% and torsional strength by 39.2% (Lesh ML, JBJS 2000;82:1096). But notching has not been shown to increase fracture risk or change clinical outcomes (Ritter MA, JBJS 2005;87:2411).
- Consider low-dose antibiotic laden cement (<2g antibiotic per 40g cement). (Bourne R, J Arthroplasty 2004;19:69).
- TKA Case card.
- Consider pain relief cocktail injection: narcotic, anti inflammatory, vaso-constrictor. 30 mg of ketorolac, 5 mg of epimorphine, 0.6 mL of 0.1% epinephrine, and 400 mg of ropivacaine, in a 100 mL volume. Due not use if using filtered blood reinfusion drains.
TKA Goals
- (1)Restore mechanical alignment [neutral tibiofemoral alignment = 4°-6° of anatomic valgus], (2)horizontal joint line, (3)soft tissue balance (ligament), (4)patella tracking (Q-angle)
TKA Keys
- Bilateral TKA: Staggered TKA(4-7 days apart in single hospitalization) has the lowest overall rate of complications for pts requiring bilateral TKA as compared to sequential TKA and staged TKA. (Sliva CD, JBJS Am 2005;87:508-513)
Valgus Deformity Considerations (valgus TKA)
- Release osteophytes & capsule >iliotibial band if tight in extension; popliteus if tight in flexion> PCL>LCL : If tight in both flexion and extension consider release LCL first and preserving other lateral stabilizers. Consider MCL advancement / reconstruction for severe valgus with medial laxity. Alternative technique for valgus knee = Elkus M, JBJS 2004:86A;2671
- Valgus deformity is generally from deformity of the distal femur rather than the proximal tibia such as hypoplastic lateral femoral condyle. Must consider any lateral condyle deformity when aligning knee to avoid internal rotation of the femoral component especially with posterior condyle line is used to position the cutting block. (Favorito PJ, Mihalko WM, Krackow KA. Total knee arthroplasty in the valgus knee. J Am Acad Orthop Surg. 2002 Jan-Feb;10(1):16-24).
- Valgus knees have: loose MCL, tight lateral retinculum, tight LCL, tight Posterolateral corner, atrophic lateral femoral condyle, lateral patellar tracking, ER of the tibia relative to the femur.
Varus Deformity Considerations
- Release osteophytes >deep MCL>posteromedial corner & semimembranosus insertion >elevation of superficial MCL> ? PCL
TKA component design
- Polyethylene must be direct-compression molded, without calcium stearate
- Want irradiation in inert environment (without air)
- Crystallinity >70% = higher wear. Want crystallinity 50-56%
- Want short shelf storage time
- 5.0% revision rate for minimally stabilized replacements compared to 6.0% posterior-stabilized replacements. (Vertullo C, JBJS 2017:99(13):1129–1139)
- Posterior Cruciate Retainingdesigns: Advantages = bone preservation, potentially more physioligic femoral rollback, PCL proprioception. Disadvantages = May cause paradoxical anterior femoral sliding instead of rollback, posterior femoral subluxation if too tight or flexion instability if too lose, late PCL laxity, less congruent joint surface with potential increased articular stress, difficult to correct severe deformities.
- PS (PCL substituting: Advantages = fixed rollback, more congruent joint surface. Disadvantages: patellofemoral clunck syndrome, rare implant dislocation, loss of proprioception, femoral notch resection needed.
- Mobile-bearing:Advantages = ultra conforming articular geometry with low contact stress, automatic rotational aligment correction. Disadvantages = potential bearing dislocation, may be technically more difficult.
- Bearing Materials: metal on metal, Alumina/Zirconia Ceramic, Polyethylene.
TKA Technique
- Pre-op: Check implants available, instruments available, reciprocating saw for notch cuts, ortho bump for initial exposure, .050 inch oscillating saw)
- supine position, ancef antibiotic
- Anesthesia: Consider peripheral nerve blocks (Horlocker TT, JAAOS 2006;14:126)
- bony prominences well padded
- foley catheter
- tourniquet high on the thigh
- r/l LE prepped and draped in standard sterile fashion
- limb exsanguinated with Esmarch, tourniquet inflated to 300mmHg
- midline incision, just above patella to just medial to tibial tubercle. With knee flexed slightly
- SQ, deep fascia
- medial parapatellar arthrotomy
- medial release
- lateral patellofemoral ligament released
- posterior half of infrapatellar fat pad
- patella everted and knee flexed
- gross arthrosis in medial compartment/lateral compartment/patellofemoral compartment
- osteophytes excised
- Proximal tibia
- intrameduallary guide
- drill hole in line with tibial shaft usally just lateral to insertion of ACL
- suction cannel to remove medullary fat
- insert fluted IM guide
- 7 3 or 0-degree tibial boom to determine posterior tibial resection
- tightened in place with boom and cutting block centered on medial 1/3 of tibial tubercle
- varus/valgus alignment varified with Extramedullary alignment arch and alignment rod. Distal end pointing to second toe.
- set resection 20mm from femoral resection, 2mm off low side or 10mm off high side and pin in place
- IM rod removed
- retractors placed to protect MCL/LCL
- transverse osteotomy of proximal tibia tilted 5 degree posteriorly
- meniscal remnants excised
- size tibia and recheck varus/valgus with alignment rod
- Femoral Cuts
- hole drilled in center of patellar sulcus of distal femur with step drill
- canal suctioned
- IM guide set to 5-7 degree of valgus with standard cut block attached and placed in IM hole
- handles positioned relative to epicondylar axis (lateral epicondyle=origin of LCL, medial=center of broad origin of MCL)
- distal femoral cutting guide attached and pinned in place
- IM rod removed
- A/P sizing rotation guide (if between sizes go smaller) insert headless pins
- 4 in 1 cut block placed and check for anterior notching, pinned in place
- posterior condyle cut
- posterior chamfer
- anterior condyle
- anterior chamfer
- reference marks scored for box cut, femoral pegs drilled
- Notch chamfer guide place and pinned, notch performed with saw and osteotome. For Zimmer box cut, mark saw blade at 30mm which is the depth of the box.
- Patella
- measure patella (25-30mm)
- patellar buttons are usually 10mm thick
- make cut restore patella height with button
- measure size
- slight medial placement
- drill patellar holes using guide
- Consider pain cocktail injection: bupivicaine 80mg, methylprednisolone 40mg, morphine 4mg, epinephrine 300mcg, cefuroxime 750mg diluted in 30 ccs of normal saline (Ranawat CS) and multimodal pain management (Peters CL, J Arthroplasty 2006;21 suppl 2:132).
TKA Complications
- Death: 0.53%
- Periprosthetic Infection: 0.71%
- Pulmonary emboli: 0.41%
- Patella fracture:
- Component Loosening:
- Tibial tray wear:
- Peroneal Nerve Palsy: 0.3% to 2%
- Periprosthetic Femur Fracture:
- Periprosthetic Tibial Fracture:
- Wound Complications / Skin slough: rare
- Patellar Clunk Syndrome: rare
- Patellofemoral Instability: 0.5%-29%
- DVT:
- Instability:
- Popliteal artery injury: 0.05%. Popliteal artery is generally posterolateral to the PCL. (Ninomiya JT, Dean JC, Goldberg VM. Injury to the popliteal artery and its anatomic location in total knee arthroplasty. J Arthroplasty. 1999 Oct;14(7):803-9.)
- Quadriceps Tendon Rupture: 0.1%
- Patellar Tendon Rupture: <2%
- Stiffness following total knee arthroplasty: deep infection should be ruled out first. Other causes of TKA stiffness are overstuffing of the patella, malpositioning of the components, ligamentous imbalance, genetic predisposition, aggressive arthrofibrosis;. Outcome of revision TKA for stiffness is poor if no reason for stiffness is determined. (Kim J, J Bone Joint Surg Am 2004;86-A(7):1479-1484.)
- Fat Embolism
- MCL rupture
- Vascular injury: asymmetrical absent pulses post-operatively: consider vascular surgery consult with intraoperative arteriogram; stent vs operative repair.
TKA Follow-up care
- TKA Rehab Protocol.
- 10-14 Days: wound check, staple removal.
- 6 weeks: review xrays.
- 3 Months: review progress with PT.
- 6 Months: review xrays, assess progress.
- 1 Year: review xrays for signs of loosening / wear.
- 2 Years: review xrays for signs of loosening / wear.
- 5 Years: review xrays for signs of loosening / wear.
- 10 Years: review xrays for signs of loosening / wear.
- Driving: may drive at 6 weeks. (Pierson JL, J Arthroplasty 2003;18:840).
- AAOS Urologic procedures in patients with THA recommendations.
- AAOS Antibiotic Prophylasis for Dental procedures.
- AAOS Post Arthroplasty Antibiotic Prophylaxis recommendations for elective procedures.
TKA Post-op Day 1
- DVT prophylaxis: Lovenox 40 mg SC once a day (initiated 12 [±3] hours preop) or 30 mg q12h SC (initiated 12 to 24 hours post op)
- Discontinue drain when output is <30cc/8hrs
- Check I’s & O’s and hep lock IV if appropriate
- Discontinue foley as soon as possible. Discontinue prophylactic Bactrim once foley is out
- Ensure SCD’s are on and working.
- Enusre patient has an incentive spirometer and understands its use.
- Anemia: Ferrous sulfate or transfusion as indicated.
- Start CPM 0-30 advance by 10 degree increments to 0-90 as tolerated.
- Order: 3-in-1 bedside cammode, elevated toilet seat and walker.
TKA Outcomes
- Survivorship: 90% at 10 years, 80% at 15 years, 75% at 20 years. (Froimson MI, OKU-8). Survivorship is decreased by: obesity, young age, male gender, malaligned prostheses, JRA, Hemophelia, osteonecrosis, patellofemoral arthritis.
- 90-95% satisfactory outcome
- 2% revision, <2% infection.
- Knee Outcome measures.
TKA Review References
- Lotke PA, Master Techniques in Orthopedics Surgery: Knee Arthroplasty, 2nd ed., 2002°
|