 |
Proximal humerus ossification centers
- The proximal humerus develops from 3 ossification centers: humeral head, greater tuberosity, and lesser tuberosity.
- Humeral head ossification center usually appears between the fourth and sixth months of life.
- Greater tuberosity ossification center usually appears during the 3 year of life.
- Lesser tuberosity ossification center usually appears during 5th hear of life
- Proximal humeral ossification centers are generally fused by age 19.
|
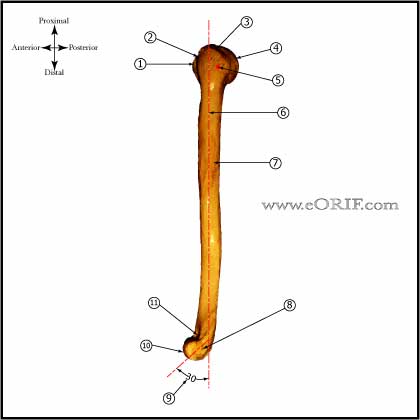 |
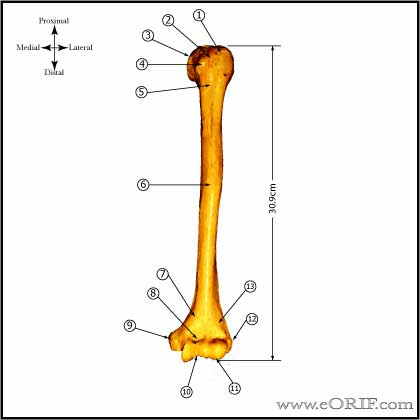
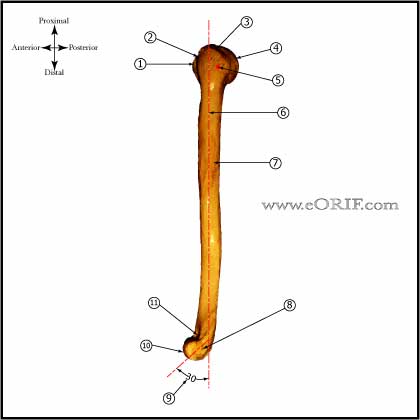
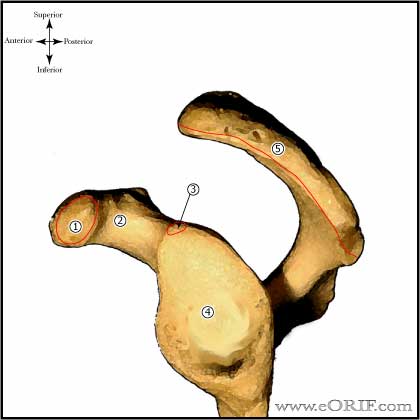
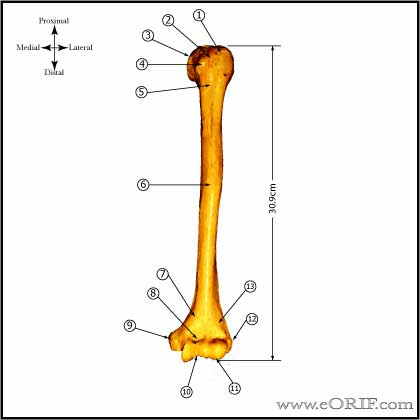
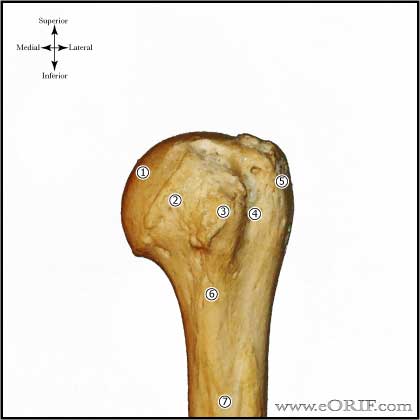
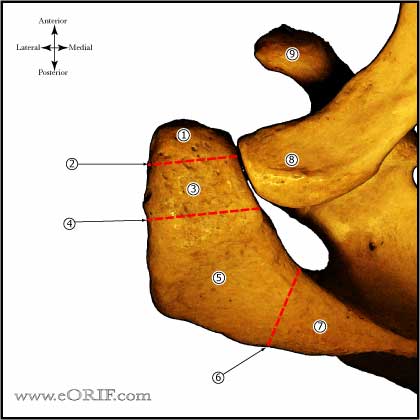
Humerus
|
 |
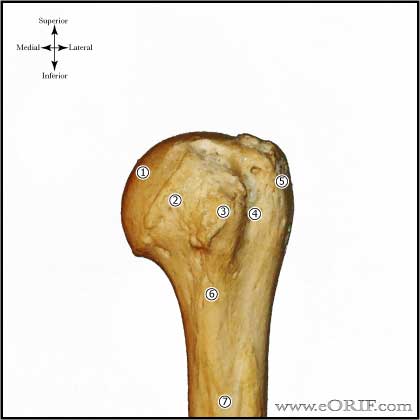
Humeral Head
- Humeral head radius averages 23mm (17-28mm) (Robertson DD, JBJS 2000;82A:1594)
- Humeral head thickness averages 19mm (15-24mm) (Robertson DD, JBJS 2000;82A:1594)
- The center of the humeral head is offset 7mm medially and 2mm posteriorly relative to the humeral axis. (Robertson DD, JBJS 2000;82A:1594)
- Humeral head inclination averages 41 degress. (Robertson DD, JBJS 2000;82A:1594)
- Neck-shaft angle averages 131 degrees. (Robertson DD, JBJS 2000;82A:1594)
- Proximal humeral retroversion averages 19 degrees, but is variable (9 to 31 degrees)
- Superior articular surface of the humeral head is usually 8-10mm superior to the highest point of the greater tuberosity.
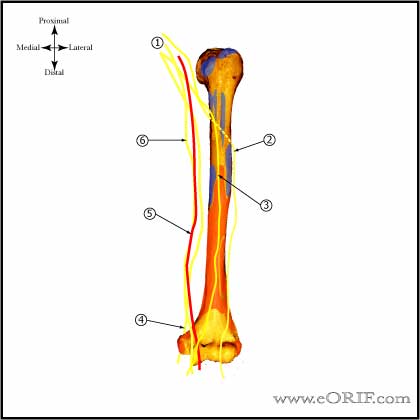
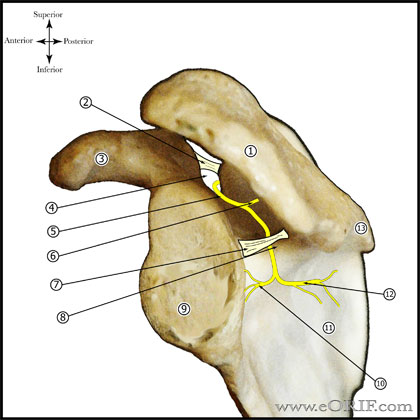
- Blood Supply: main source is the anterolateral (arcuate) branch of the anterior humeral circumflex artery, which runs under the long head of the biceps tendon and then adjacent to the lateral aspect of the intertubercular groove. It enters the humeral head at ehr proximal end of the transition from the greater tuberosity to the intertubercular groove. (Gerber C, JBJS 1990;72A:1486)
|
 |
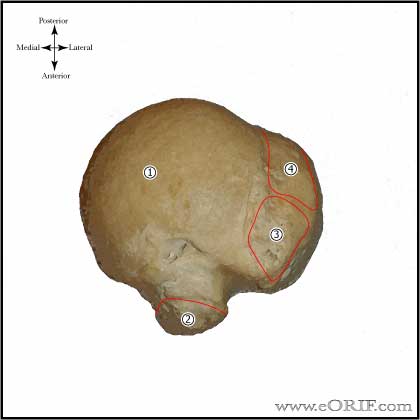
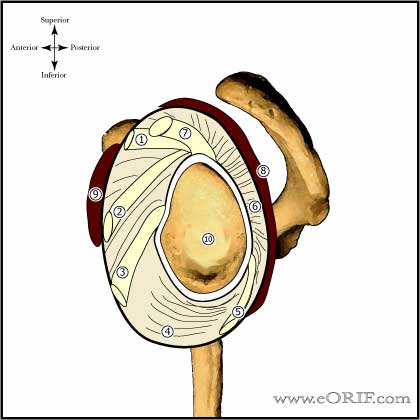
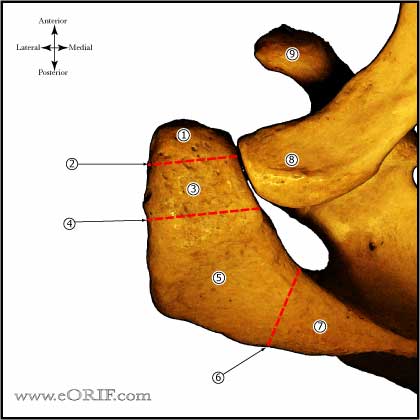
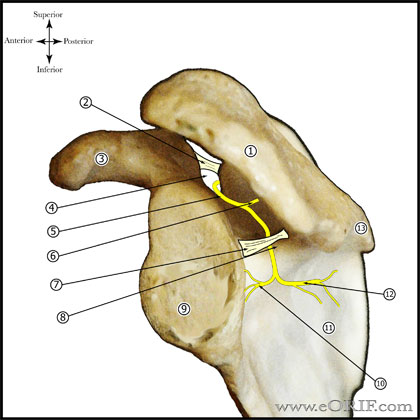
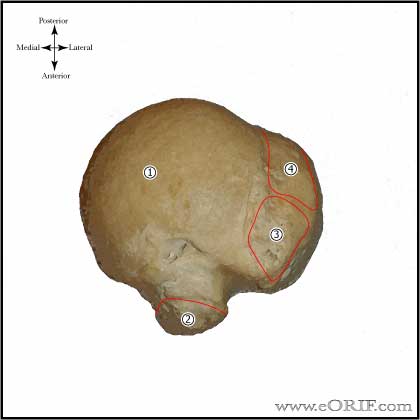
Glenoid Anatomy
- Articular surface is concave. The hyaline cartilage covering the glenoid is thicker toward the periphery and thinner in the center.
- Glenoid inclination is variable, but averages @4.25 degrees superior (range -7 to 15.8) (Churchill RS, JSES 2001;10:327)
- Glenoid version averages 1.23 degrees of retroversion (Churchill RS, JSES 2001;10:327)
- Glenoid width averages 28.8 +/- 1.6mm in males and 23.6 +/- 1.5mm in females. (Churchill RS, JSES 2001;10:327)
- Glenoid height averages 37.5 +/- 2.2mm in males and 32.6 +/- 1.8mm in females. (Churchill RS, JSES 2001;10:327)
- Radius of curvature of the glenoid in the coronal plane averages 2.3mm greater than that of the humeral head, but because the cartilage is thinner in the center of the glenoid with radius of curvature for the glenoid and humeral head including their cartilage surfaces is nearly equal.
- Vascularity: (Cooper DE, JBJS 1992;74A:46).
|
|
Superior Glenohumeral Ligament (SGHL)
- Origin: glenoid labrum near the long head of the biceps tendon origin.
- Insertion: just superior to the lesser tuberosity.
- Present in 94% generally with a diameter >2mm, although size is variable. (Steinbeck J, JSES 1998;7:122).
- Primary restraint to inferior subluxation when the arm is in adduction (Turkel SJ, JBJS 1981;63A:1208).
- Limits anterior translation and combined inferior translation and external rotation when the arm is in adduction. (Burkart AC, CORR 2002;400:32).
- Superior glenohumeral ligament and coracohumeral ligament are the primary restraints to posterior translation with the are flexed, adducted and internally rotated.
- (O'Brien SJ, AJSM 1990;18:449), (Warner JJ, AJSM 1992;20:675).
|
|
Middle Glenohumeral Ligament
- Origin: glenoid labrum just below the SGHL.
- Insertion: humerus just medial to the lesser tuberosity.
- Present in 85%; average3.6mm diameter, although quite variable in size. (Steinbeck J, JSES 1998;7:122)
- Prevents anterior translation in the 45° abducted shoulder and limits external rotation. Limits anterior-posterior translation when the humeral head is in 60°-90° of abduction and external rotation, limits inferior translation with arm in adduction (Warner JJ, AJSM 1992;20:675).
- (O'Brien SJ, AJSM 1990;18:449), (Warner JJ, AJSM 1992;20:675).
|
 |
Inferior Glenohumeral Ligament
- Origin: glenoid labrum from the 3 o'clock to 9 o'clock postion. Consists of a thick anterior band and a thin posterior band.
- Insertion: just below the articualr margin of the humeral head.
- Present in 72%; anterior band averages 2.8mm in diameter; posterior band averages 1.8mm in diameter.
- Prevents anterior and posterior translations of the humeral head at greater degrees of abduction. Secondary restaint to inferior translation in the abducted shoulder.
- Anterior band of the IGHL is the primary restraint to anterior translation at 90° abduction
- Posterior band of the inferior glenohumeral ligament complex is the primarly restraint to posterior translation with the arm in abduction.
- (O'Brien SJ, AJSM 1990;18:449), (Warner JJ, AJSM 1992;20:675).
|
| |
Coracohumeral Ligament
- Thick band of fibrous tissue extending from the coracoid process to the tuberosities between the supraspinatus and subscapularis tendons.
- Deep to the RTC tendon insertions, blends with the capsule and supraspinatus to form part of the roof of the biceps sheath. . (Clark, JBJS 1992;74A:713)
- Origin: lateral surface of the coracoid process.
- Insertion: greater and lesser tuberosities adjacent to the bicipital groove.
- Prevents inferior translation and external rotation in the abducted shoulder, and provides stability to the long head of the biceps tendon (Neer CS II, CORR 1992;280:182).
- Superior glenohumeral ligament and coracohumeral ligament are the primary restraints to posterior translation with the arm flexed, adducted and internally rotated.
- (Edelson JG, JBJS 1991;73Br:150).
- Fealy S, JSES 2005;14:542
|
| |
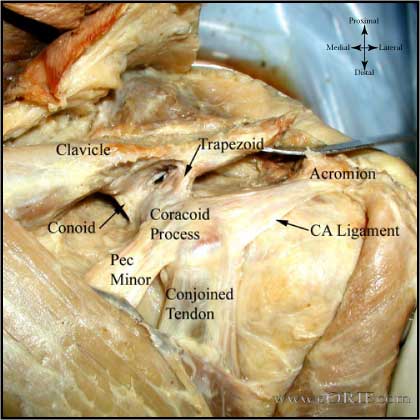
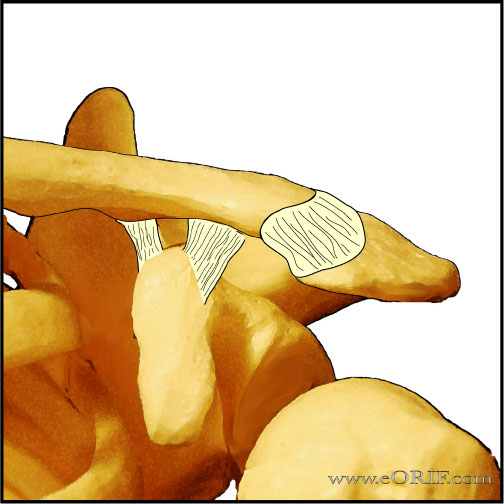
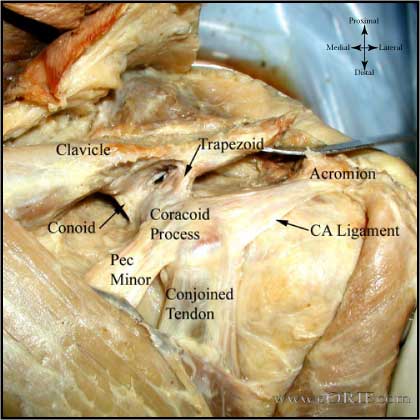
Coracoacromial ligament (CAL)
- Origin: arises as a 32mm band on the coracoid process.
- Insertion: inserts along 19mm of the anterior acromion.
- Thickness: 1.3mm at its midpoint.
- Consists of an anterolateral and posteromedial band. (Fealy S, JSES 2005;14:542)
- Functions as a superior restaint to humeral translation and is under a 20N at rest in situ.
- Prevents anterosuperior translation / escape in patients with massive RTC tears.
- Must not be disrupted in patients with RTC tears. (Arntz CT, J Arthroplasty 1991;6:363).
|
| |
Coracoacromial Arch
- formed by the coracoacromial ligament and coracoid anterioly and the acromion posteriorly.
|
|
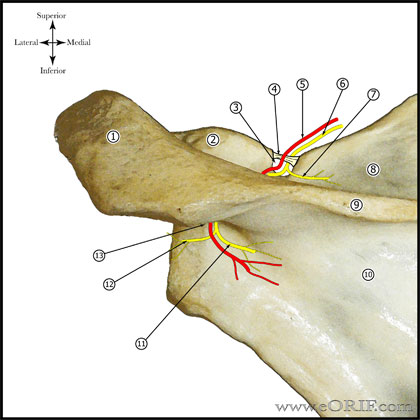
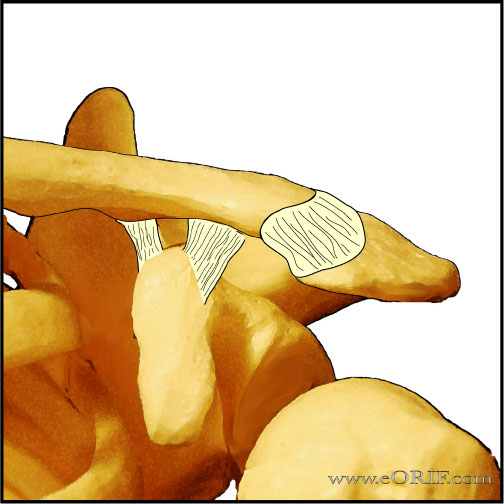
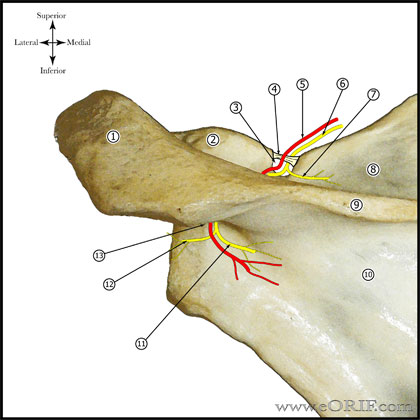
Acromioclavicular Ligament Anatomy
- AC joint is a diathrodial joint with a fibrocartilaginous disk. The disk has a great variation in size and shape and eventually undergoes rapid degeneration until it is essentially non-functional by the fourth decade.4
- AC joint is surrounded by a thin capsule reinforced by the acromioclavicular and coracoclavicular ligaments.
- AC ligaments stabilize the joint in the anteroposterior direction.5,6 The superior AC ligament is the stongest of the AC ligaments. Its fibers blend with the fibers of the deltoid and trapezius muscles. Distal clavicle resection, which is part of many described treatment methods, leads to anteroposterior instability due to loss of the AC ligaments.7 The posterior and superior AC ligaments should be preserved during distal clavicle resection to prevent posterior instability. (Klimkiewicz JJ, JSES 1999;8:119)
- Coracoclavicular ligament is made up of the trapezoid and conoid ligament. It is the prime suspensory ligament of the upper extremity.8
- Trapezoid ligament in men has a mean length of 1.61 +/- 0.52 and a width of 1.58 +/-0.69 cm.5 Orgin = coracoid process, anterior and lateral to the attachment of the conoid ligament. Insertion = a rough line on the undersurface of the clavicle extending anteriorly and laterally from the conoid tubercle. Trapezoid ligament is the primary restraint to axial compressive force on the AC joint.
- Conoid ligament in men has a mean length of 1.225 +/- 0.658 cm and width of 0.737 +/-0.148 cm.5 Origin = the posteromedial side of the base of the coracoid process. Insertion = conoid tubercle on the posterior undersurface of the clavicle. The conoid tubercle is located at the apex of the posterior clavicular curve, which is at the junction of the lateral third of the flattened clavicle with the medial two thirds of the triangular-shaped shaft.
- Based on available anatomic studies9,10obvious oversimplifications can be made: the AC ligaments control anteroposterior stability, the CC ligaments control superoinferior stability.
- The deltoid and trapezius are also important in supplying dynamic stability to the AC joint.11
- average space between coracoid and clavicle is 1.1 to 1.3cm
|
| |
Subacromial bursa
- Lines the anterior half of the acromial undersurface.
- Contains numerous free nerve endings which may be responsible for shoulder pain.
|

|
Labrum
|
| |
Rotator Interval Anatomy
- The RI is a triangle shaped region between the supraspinatus and supscapularis tendons. The base is the coracoid process. The apex is the intertubercular groove. The inferior border is the superior aspect of the subscapularis tendon. The superior border is the anterior aspect of the supraspinatus tendon.
- Contents of RI = long head of biceps tendon, superior glenohumeral ligament, glenohumeral capsule, and the coracohumeral ligament. (Bennett WF, Arthroscopy 2001;17:101)
- Rotator interval release leds to dislocaiton in 50% of specimens (occurs in 60° of abduction and external roation. (Fitpatrick MJ, Arthroscopy 2003;19(suppl1):70).
|
| |
Rotator Cuff Anatomy
- The tendons of the rotator cuff muscles fuse into one structure at or near their tuberosity insertions.
- Supraspinatus and infraspinatus tendons join about 15mm proximal to their insertion and become inseparable. (Clark, JBJS 1992;74A:713)
- The teres minor and subscapularis have muscular insertions on the surgical neck of the humerus that extend @2cm inferior to the tendinous attachment.
- The subscapulanis and supraspinatus tendons fuse to form a sheath that surrounds the biceps tendon at the proximal end of the bicipital groove. A tendinous slip extends anterolaterally from the supraspinatus tendon to form the roof of the sheath. The superior part of the subscapularis tendon passes under the biceps tendon for @7mm to form the floor of the sheath.(Clark, JBJS 1992;74A:713)
- Layers of RTC (in area of supraspinatus/infraspinatus) (Clark, JBJS 1992;74A:713)
-Layer 1: superficial extension of the coracohumeral ligament overlying the cuff tendons and extending from the coracoid process to the greater tuberosity.
-Layer 2: supraspinatus and infraspinatus fibers oriented parallel to the axes of the tendons
-Layer 3: smaller supraspinatus and infraspinatus fibers which are smaller and obliquely oriented with respect to Layer 2 fibers. Supraspinatus tendon fans out, intermingling with the fibers of the infraspinatus and subscapularis.
-Layer 4: deep extension of the coracohumeral ligament
-Layer 5: true joint capsule of the shoulder, extending from the glenoid labrum to the neck of the humerus.
- Subscapularis: area= 2.41 cm2 ; Sup/Inf= 2.43 cm; M/L=1.79 cm (Dugas JR, JSES 2002;11:498).
- Supraspinatus: area=1.55 cm2 M/L=1.27: A/P=1.63 cm (Dugas JR, JSES 2002;11:498).
- Infraspinatus: area= 1.76; M/L=1.34 cm; A/P= 1.64 (Dugas JR, JSES 2002;11:498).
- Teres minor: area= 2.22 cm2; M/L=1.14 cm; A/P=2.07 (Dugas JR, JSES 2002;11:498).
- Mean total area of insertion of the rotator cuff tendons onto the greater tuberosity = 5.53 cm2.(Dugas JR, JSES 2002;11:498).
|
 |
Long Head of Biceps Tendon
- Originates from the supraglenoid tubercle (30%), Glenoid labrum (45%), or supraglenoid tubercle and glenoid labrum (25%)
- Average length = 102mm
- Long head of the biceps tendon functions as a humeral head depressor and is a secondary restraint to anterior instability, particularily in the abducted/internally rotated position (Kumar VP CORR 1989:244:172).
- Stabilizing ligamentous pulley of the biceps consists of the confluence of the superior glenohumeral ligament and the coracohumeral ligament with fibrous contributions from the subscapularis and supraspinatus tendons. (Bennett WF, Arthroscopy 2001;17:173).
- The biceps tendon contains a large network of sensory and sympathetic nerve fibers, mainly at its insertion. (Alpantaki K, JBJS 2005;87A:1580).
- Intra-articular displacement of the biceps tendon indicates subscapularis rupture.
- Biceps tenotomy significantly improves pain in patients with massive RTC tears. (Walch G JSES, 2005;14:238).
- see Biceps Tendonitis; Biceps Tenodesis technique; Proximal biceps tendon rupture.
|
| |
Anterior Humeral Circumflex Artery
- provides blood supply to the majority of the humeral head via the anterolateral ascending branch of the aneriro circumflex humeral artery. The terminal branch is termed the arcuate artery.
- Gerber D, JBJS 1990;72A:1486
|
 |
Acromion
- Size in men: Average length = 48.5mm; average anterior width = 19.5mm, average anterior thickness = 7.7mm (Nicholson GP, JSES 1996;5:1)
- Size in women: Average length = 40.6mm; average anterior width = 18.4mm, average anterior thickness = 6.7mm (Nicholson GP, JSES 1996;5:1)
- Acromial facet of AC joint morphology: 49% medially inclined (superolateral to inferomedial); 48% vertical; 3% laterally inclined.
- Acromial morphology: the undersurface of the anterior acromion is classified as flat (type 1), curved (type II) or hooked (type III) based on outlet vew lateral xrays.
- Serves as site of origin of the deltoid muscle and the AC joint ligaments.
- Os acromionale (unfused secondary ossification center) has 3% incidence. 60% will be bilateral.
|
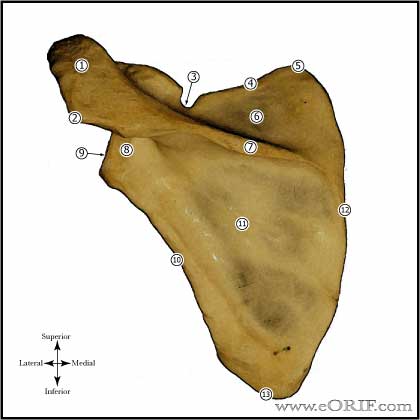 |
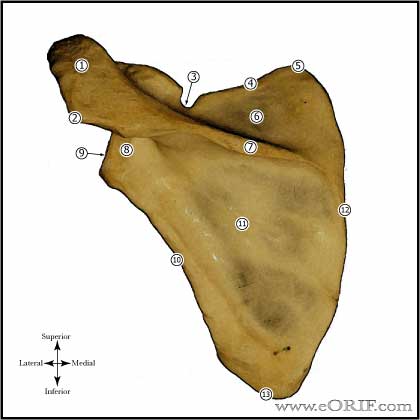
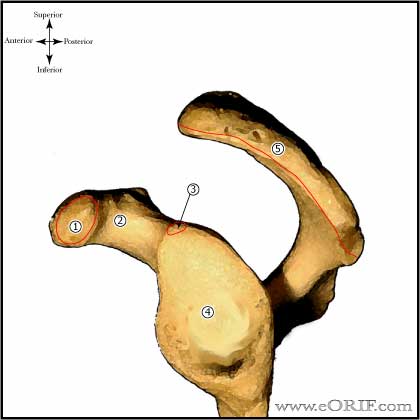
Scapula
- Serves as insertion site for 17 muscles
- Consists of the body, coracoid process and acromion.
|
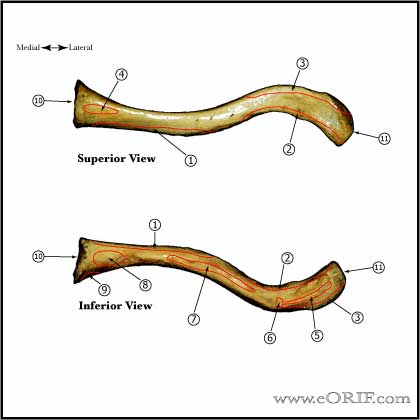 |
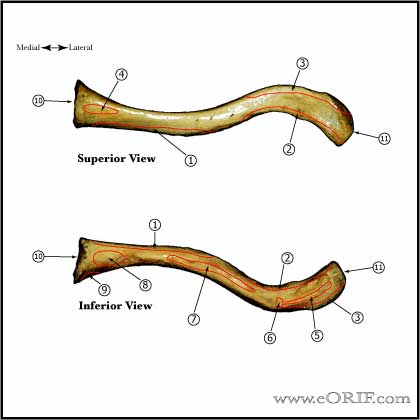
Clavicle Anatomy
- First bone to ossify, 5thgestational wee
- Only long bone to ossify be intramembranous ossification
- Medial physis=80% of longitudinal growth
- Both acromial and sternal physes can remain open into 3rddecade of life
- Middle 1/3 fractures typically heal with the lateral shaft fragment displaced posterior to the medial shaft fragment / anterior-posterior angulation. (Edleson JG, JSES 2003;12:173).
- See also Clavicle Fracture.
|
| |
Scapulothoracic Articulation
- (Williams GR, CORR 1999;359:237)
|
| |
|
| |
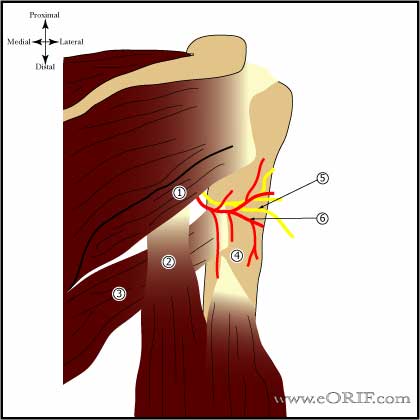
Deltoid Muscle
- Consists of three parts: anterior, middle or lateral, and posterior.
- Origin: Anterior deltoid = superior and anterior surfaces of the lateral third of the clavicle and the acromion. Lateral = superior and lateral acromion. Posterior deltoid = posterior-inferior border of the scapular spine.
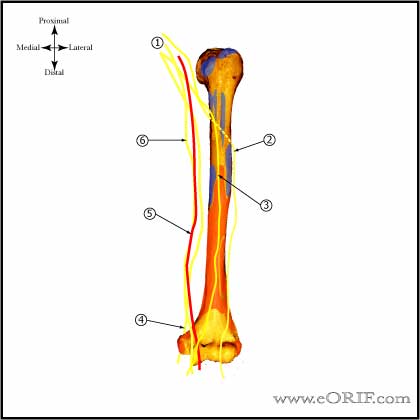
- Insertion: the deltoid tuberosity on the lateral aspect of the humerus. Mean length of the deltoid insertion = 97mm. The mean distance from the greater tuberosity to the proximal insertion point = 61mm. Distal insertion = 158mm. The deltoid occupies on average: 8% of the humeral circumference 5 mm from the proximal insertion point, 39% at the mid point of the insertion, and 31% of the humeral circumference 5 mm from the distal insertion point. (Morgan SJ, JOT 2006;20:19), see also (Rispoli D, JSES 2009;18:386)
|
| |
NERVES |
 |
Brachial Plexus Anatomy
- Brachial plexus is formed from C5, C6, C7, C8, and T1 nerve roots. There may be contributions from C4, and T2. A plexus with contributions from C4 is called “prefixed.” (28% to 62%). "Postfixed" = contributions from T2 (16% to 73%). (KerrAT, AmJ Anat 1918;23:285).
- Roots and trunks are more commonly affected than the divisions, cords, or terminal branches.
- Trapezius and levator scapulae muscles are almost always intact after traumatic brachial plexus injury allowing for active arm abduction through the scapulothoracic articulation.
- If serratus anterior function is preserved, forward elevation of the arm through scapular rotation is possible.
- Preganglionic injury = spinal roots are avulsed from the spinal cord; little potential for recovery. Postganglionic = distal to the dorsal root ganglion; some potential for spontaneous recovery.
- Avulsion of the T1 root (a pre-ganglionic injury) interrupts the T1 sympathetic ganglion,causeing Horner's syndrome (miosis (small pupil), enophthalmos (sinking of the orbit), ptosis (lid droop), and anhydrosis (dry eyes).
- Injury to C5,C6,C7 may result in loss of shoulder flexion, elbow fexion and extension and occasionally wrist and finger extension.
- Injury to C8 and T1 may limit hand function.
- See Brachial Plexus palsy.
|
| |
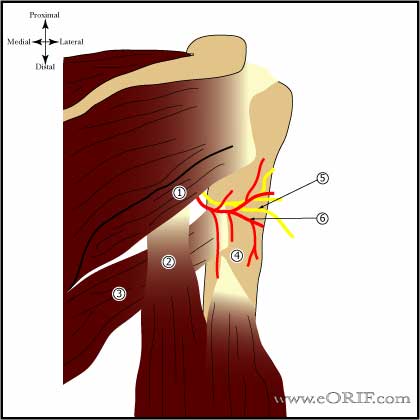
Axillary Nerve
- Terminal branch of posterior cord derived from ventral rami C5&6
- Runs anterior to subscapularis
- Enters quadrilateral space with posterior humeral circumflex artery
- In contact with inferior joint capsule.
- Branches into anterior trunk{ant 2/3 deltoid} and posterior trunk{post 1/3 deltoid,teres minor}
- Anterior trunk lies 4-7cm inferior to anterolateral acromion.
- Motor innervation: deltoid, teres minor
- Sensory innervation: lateral aspect of shoulder and brachium in a chevron distribution.
- Arthroscopic visualization of the axillary nerve (Paribelli G, Arthroscopy 2005:21:1016).
- Bono CM, CORR 2000;373:259
- Burkhead WZ, JSES 1992;1:31
- see also Axillary Nerve Palsy.
|
|
Suprascapular nerve
- Origin: Upper trunk of brachial plexus (C5, C6).
- Innervation: Mixed peripheral nerve with motor supply to the supraspinatus and infraspinatus and sensory innervation to the posterior joint capsule. No cutaneous sensory innervation.
- Passed beneath the superior transverse scapular ligament. Suprascapular artery passes above the superior transverse scapular ligament.
- At risk during the posterior interval slide.
- Curves tightly around the base of the scapular spine at its junction with the posterior glenoid neck, enveloped within a fat pad.
- The average distance from the origin of the long tendon of the biceps to the motor branches of the supraspinatus is 2 cm. The average distance from the posterior rim of the glenoid to the motor branches of the infraspinatus muscle is 2cm. (Warner JJP,JBJS 1992; 74Am: 36-45)
- See also Suprascapular Nerve Palsy.
- (Bibliani LU, Arthroscopy 1990;6:301),
|
 |
Musculocutaneous nerve
- Origin:
- Termination: becomes the lateral antebrachial cutaneous nerve.
- Runs under the conjoined tendon distal to the coracoid process. At risk of injury during during open shoulder procedures, generally from vigorous retraction.
- Motor: biceps, coracobrachiaolis, medial half of brachialis
- Sensation:
- See also Musculcutaneous nerve palsy.
|
| |
Median nerve |
| |
Radial Nerve
- Origin: Posterior Cord of brachial plexus
- Terminatial branch:
- Travels along spiral groove of humerus.
- Branches into posterior interosseous nerve, superficial radial nerve and posterior cutaneous nerve at the level of the lateral humeral condyle.
|
| |
Ulnar Nerve |
| |
Medial Antebrachial cutaneous nerve |
| |
Lateral Antebrachial cutaneous nerve.
- Origin: terminal branch of the musculocutaneous nerve
|
| |
Long Thoracic Nerve
- Formed by branches of the C5, C6, and C7 nerve roots. C5 and C6 branches join beneath the scalenus medius muscle forming the upper division of the long thoracic nerve, located 1 cm posteriorly and superiorly to the upper trunk origin.
- The upper division joins the branch from C7 caudally, in the axillary region.
- Innervates the serratus anterior muscle
- Bertelli JA, JBJS 2005;87A:993
|
| |
Arteries and Veins |
| |
Cephalic Vein |
| |
Brachial Artery |
| |
Anterior Humeral Circumflex Artery
- Runs along the inferior border of the subscapularis
- Injury may lead to avascular necrosis of the humeral head.
|
 |
Posterior Humeral Circumflex Artery
- Provides blood supply to the posterior portion of the greater tuberosity and a small posteroinferior portion of the humeral head.
- Gerber D, JBJS 1990;72A:1486
- May become occluded in the Quadrilateral Space.
|
| |
Shoulder Ossification Centers
- Clavicle
Medial: forms during 5th week of gestation
Lateral: forms during 5th week of gestation
- Coracoid Process:
Center: forms at 1 year
Base: forms at 10 years
Tip: forms during puberty
- Acromion: form during puberty
- Glenoid
Inferior: forms 1 years
Superior: forms during puberty
- Proximal humerus
Humeral head: forms at 1 year
Greater tuberosity: forms at 3 years
Lesser tuberosity: forms at 5 years
|
| |
|
| |
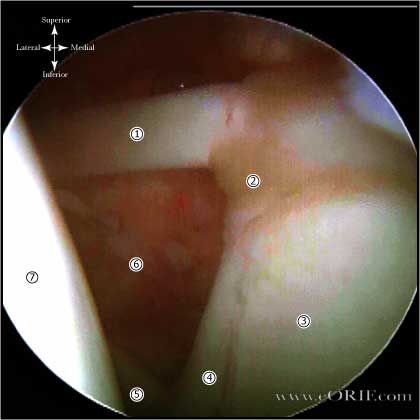
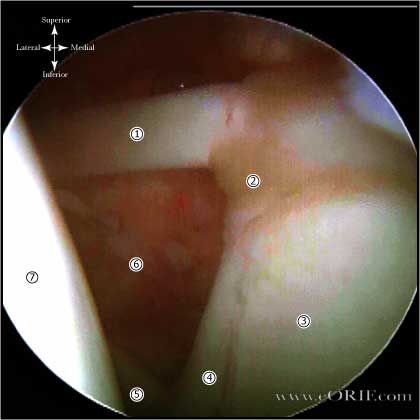
Shoulder Arthroscopy Anatomy |
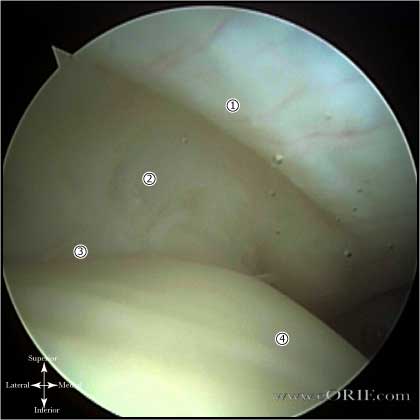 |
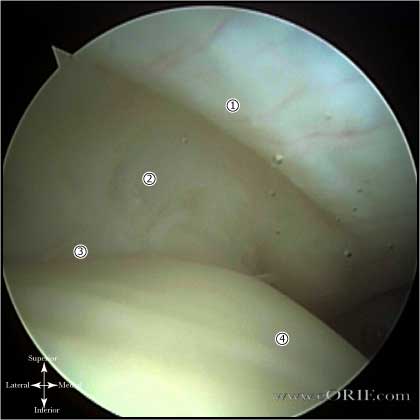
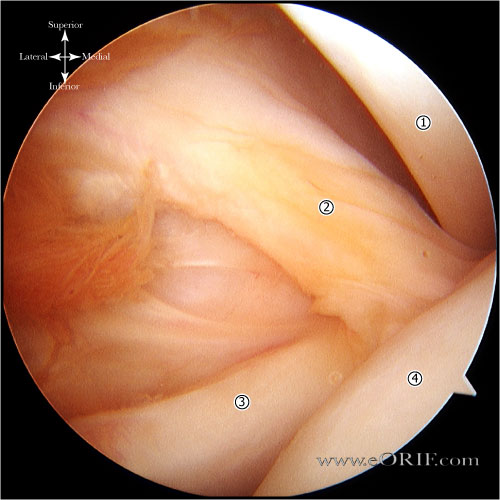
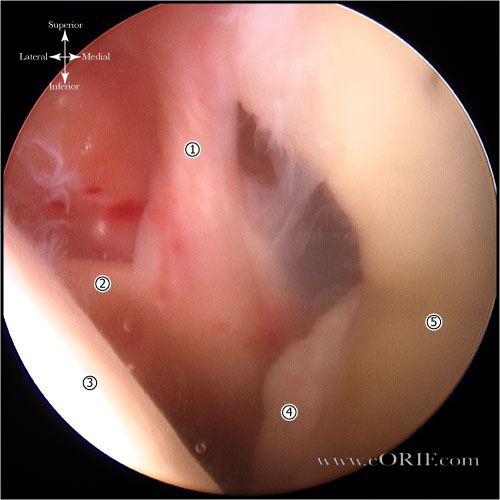
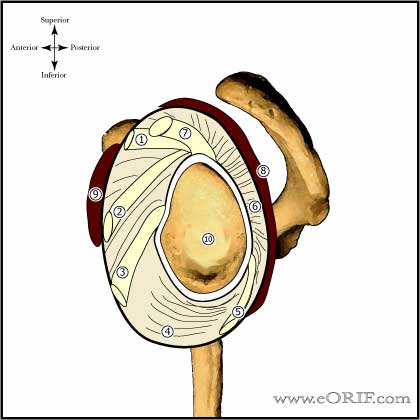
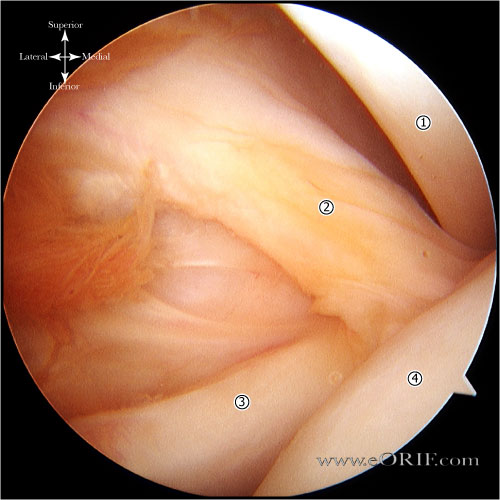
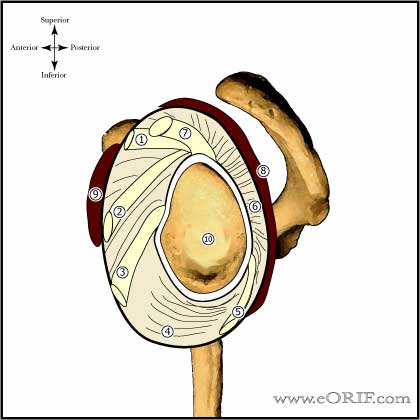
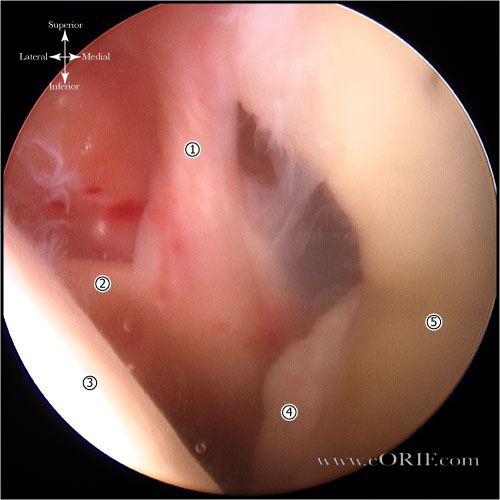
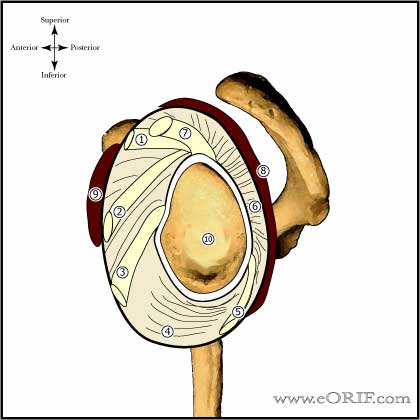
Normal RTC / Rotator Cable
- Rotator Cable: an arching, cable-like thickening of the RTC. The rotator cable averages 4.72mm in thickness which is 2.59 times the thickness of the rotator crescent that it surrounds and functions to stress-shield the rotator crescent. (Burkhart SS, Arthroscopy 1993; 9: 611-616)
- Rotator Crescent: thinner crescent of tissue that inserts into the greater tuberosity. Average size = 41.35mm (greatest A/P dimension) by 14.08mm (greatest M/L dimension).
- Greater tuberosity insertion
- Humeral head
Arthroscopic view from posterior portal in beach chair postition.
|
| |
|
| |
|
| |
|