|
|
synonyms: posterolateral corner injury, PLC injury, PLC tear, Posterolateral corner tear,
Posterolateral Corner ICD-10
Posterolateral Corner Etiology / Epidemiology / Natural History
- Posterolateral Complex includes: biceps tendon, iliotibial band, popliteus tendon, popliteofibular ligament, arcuate ligament and the LCL. (OKU-8)
- Occurs in 6%-10% of patients with acute knee hemarthrosis
- Natural history: Chronic Grade III posterolateral instability is thought to lead to persisting severe or gross lateral laxity, muscle weakness, and posttraumatic osteoarthritis of the injured knee.
Posterolateral Corner Anatomy
- Posterolateral Complex includes: biceps tendon, iliotibial band, popliteus tendon, poplitoefibular ligament, arcuate ligament and the LCL. (OKU-8)
- Some also consider it to include: the middle third of the lateral capsular ligament, the fabellofibular ligament, the posterior horn of the lateral meniscus, the lateral coronary ligament, and the posterolateral part of the joint capsule. (Covey D, JBJS 2001;83A:106-118)
- PLC Function: restraint to posterior tibial translation, varus rotation and external tibial rotation.
- Majority of injuries are distally based disruption of tissues from fibula and proximal lateral tibia.
- LCL insertion: posterior (4.6 mm) and proximal (1.3 mm) to the lateral epicondyle of the femur and posterior (8.1 mm) to the anterior point of the head of the fibula. On the femur, the popliteus tendon inserts distally (11 mm) and either anterior or posterior (mean 0.84 mm anterior) to the lateral collateral ligament. The popliteofibular ligament inserts distal (1.3 mm) and anterior (0.5 mm) to the tip of the styloid process of the fibula. (Brinkman JM, JBJS 2005;87Br:1364).
Posterolateral Corner Clinical Evaluation
- Most comonly due to hyperextension varus injury, often from direct blow to anteromedial tibia. Generally athletic injuries, MVA, or falls.
- Pain in PLC of knee. Buckling into hyperextension. Chronic injuries may have pain in medial side of knee
- Dial Test (Tibial External Rotation): Prone postion. Measure thigh-foot angle with external rotation stress applied both at 30° and 90°. Compare to normal side. External rotation of the tibia >10° compared to normal side indicates posterolateral corner injury. Increased ER at 30° but not at 90° indicates isolated posterolateral corner injury. Increased ER at both 30° and 90° indicates combined PLC, PCL injury. (Bleday RM, Arthroscopy 1998;14:489-94) (Larsen MW, J Knee Surg 2005;18:146-50).
- Posterolateral external rotation test: Posterior tanslation and external rotation forces are applied to the knee at 30° of flexion. Posterolateral subluxation of the proximal tibia indicates PLC injury.
- External rotation recurvatum test: Lift the patients extended leg by the great toe and observe for any side to side differences in hyperextension, varus and tibial external rotation. (Hughston JC, CORR 1980;147:82-7).
- Other tests for PLC laxity: Posterolateral drawer test(Hughston JC, CORR 1980;147:82-7), adduction stress test, dynamic posterior shift test, Reverse pivot shift test.
- Evaluate gait for varus thrust / varus alignment.
- Varus Stress Test: Apply varus load to knee at 0 and 30° of flexion. Increased laxity as compated to normal side indicates lateral collateral ligament injury. Instability at 30° indicates isolated LCL injury. Instability at 0° indicates combined cruciate/LCL injury.
- Lack of contained effusion is strongly predictive of complete posterolateral corner injury
- Evaluate for palpable biceps femoris tear / LCL in figure-4 position.
- Isolated PCL injury = increased posterior translation, ER(>10 degrees) and varus that is most notable at 30° flexion but not at 90° as compared to normal side.
- Combined PCL/posterolateral corner injuiry has increasing posterior translation, ER(>10°) and varus at 30° flexion and 90° as compared to normal side.
- Combined ACL/posterolateral corner injury has increased anterior and posterior translation, varus and ER as compared to normal side.
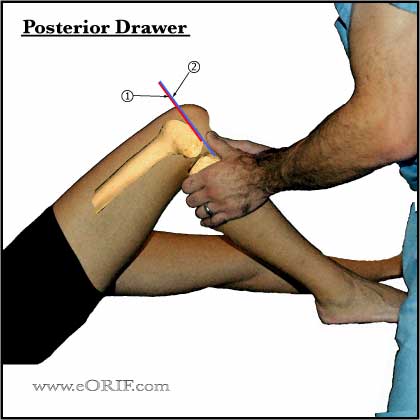
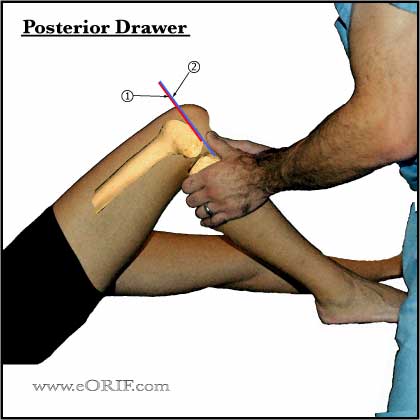
- Posterior Drawer Test: apply posterior stress to proximal tibia with knee flexed 30 degrees and 90°. Slightly increased posterior translation at 30 but normal posterior translation at 90° indicates posterolateral corner injury. Increased posterior translation at both 30 and 90° indicates PCL injury. (Grood ES, JBJS 1988;70A:88-97).Posterior drawer may also be performed with the tibial in external rotation. Always compared to normal side.
- Evaluate for Peroneal Nerve Palsy
- Document vascular status of leg (dorsalis pedis / posterior tibial pulses).
- Evaluate for ACL, MCL, LCL, PCL stability/tears
Posterolateral Corner Xray / Diagnositc Tests
- A/P, lateral, sunriseviews of knee. May be normal or show widening of the lateral joint space, arcuate fracture of the fibular head, avulsion of Gerdy's tubercle off the tibia, or Segond fracture(avulsion of capsule from lateral tibial plateaus usually associated with ACL tears)
- Standing scanogram from hip to ankle should be obtained in there is concern for malalignment. Isolated soft-tissue procedures for posterolaterial instability are likely to fail in the setting of varus alignment. (Noyes FR, Am J Sports Med 1996;24:415)
- MRI: bone contusion MFC, LCL tear, uncontained effusion, ACL/PCL tear. (LaPrade RF, AJSM 2000;28:191). Thin-sliced coronal oblique T1 images of the fibular head are best for detecting LCL, popliteus, biceps and popliteofibular ligament injury.
Posterolateral Corner Classification / Treatment
- Grade I and Grade II injuries: may be treated non-operatively with early mobilization and expected good outcomes. (Kannus P, Am J Sports Med. 1989;17:83-8). 3-wks of immobilization in full extention followed by progessive ROM and strengthening exercises.
- Grade III injury = direct repairwithing 2weeks, the sooner the easier.
- Chronic PLC injury (>3 weeks from injury): PCL reconstruction; consider Achilles/patellar tendon allograft reconstruction of popliteus and LCL; biceps femoris central section turndown LCL reconstruction. (Veltri DM, Clin Sports Med. 1994;13:615-27)
- Chronic PLC instability with varus knee alignment: Treatment = valgus-producing HTO (medial opening wedge). Soft tissue reconstructions will eventually stretch out and fail if alignment is not corrected. (Naudie DD, AJSM 2004;32:60).
- PCL / PLC injury: acute PCL Reconstruction / Posterolateral Corner Reconstruction.
- ACL /PLC injury: acute ACL Reconstruction / Posterolateral Corner Reconstruction.
- Acute Multiple ligament knee injury / Knee Dislocation
Treatment: concomitant ligament repair/reconstruction of all injuries.
PLC Technique
- Knee EUA
- Knee scope, evaluate lateral compartment for associated meniscal/chondral injury
- Measure lateral joint opening with a calibrated nerve hook. Knees that have insufficient posterolateral structures will demonstrate 8mm of joint opeing at the intercondylar notch and >12mm of opening at the periphery of the lateral compartment. (Noyes FR, in Orthoppaedic Sports Medicine, 2003;1907)
- Repair any cruciate ligament injury first
- Evaluate iliotibial tract, biceps femoris, peroneal nerve, LCL, popliteus, popliteofibular ligament.
- Repair injured structures by direct suture, sutures through drill-holes, or suture anchors.
Posterolateral Corner Associated Injuries / Differential Diagnosis
- Peroneal nerve palsy: approximatelty 15%; decreased sensation over the dorsum of the foot or weakness in ankle dorsiflexion and foot eversion.
- Meniscal Tear: medial more common
- ACL tear
- PCL Tear
- Chondral injury
- Patellar Dislocation
- Knee Dislocation
- Vascular injury
Posterolateral Corner Complications
- Peroneal nerve palsy
- Infection
- Hematoma
- Stiffness / decreased ROM
- Persistent laxity
- Painful hardware
Posterolateral Corner Follow-up Care
- Post-op: NWB, hinged knee brace locked in extention.
- 7-10 Days: Wound check, NWB, Hinged brace open from 0-45°. Begin PT, avoid hamstring activity.
- 6 Weeks: Advance to weight bearing as tolerated, Hinged brace 0-120°. Discontinue brace at 8weeks.
- 3 Months: Advance to stregthening program
- 6 Months: sport specific rehab.
- 1Yr: Return to full activities.
Posterolateral Corner Review References
|