|
|
synonyms: total joint infection, total knee infection, total hip infection, antibiotic beads
Periprosthetic Infection ICD-10
A- initial encounter
D- subsequent encounter
S- sequela
Infected TJA, irrigation and debridement only CPT Code:
- 27030, Arthrotomy, hip, with drainage (e.g., infection)
- 27310, Arthrotomy, knee, with exploration, drainage, or removal of foreign body (e.g., infection)
Infected TJA, irrigation and debridement and antibiotic bead placement CPT Code:
- 27030 and +20704
- 27310 and +20704
Infected TJA with irrigation and debridement and modular component exchange CPT Code:
- Code 27134-52, Revision of total hip arthroplasty; both components, with or without autograft or allograft, with modifier 52, Reduced Services
- Code 27486-52, Revision of total knee arthroplasty, with or without allograft; 1 component, with modifier 52, Reduced Services
Infected TJA with irrigation and debridement and modular component exchange and antibiotic bead placement CPT Code:
- 27134-52 and +20704
- 27486-52 and +20704
Revision THA with revision of a single modular articular component CPT Code:
- Code 27137-52, Revision of total hip arthroplasty; acetabular component only, with or without autograft or allograft, with modifier, Reduced Services Code 27138-52, Revision of total hip arthroplasty; femoral component only, with or without allograft, with modifier 52, Reduced Services
Revision THA with revision of a single modular articular component and antibiotic bead placement CPT Code:
- 27137-52 and +20704
- 27138-52 and +20704
Complete removal of an infected TJA resection arthroplasty with placement of an intra-articular drug-delivery device as a planned staged procedure CPT Code:
- 27091, Removal of hip prosthesis; complicated, including total hip prosthesis, methyl methacrylate with or without insertion of spacer
- 27488, Removal of prosthesis, including total knee prosthesis, methyl methacrylate with or without insertion of spacer, knee
Periprosthetic Infection Etiology / Epidemiology / Natural History
- TKA = 0.71% (SooHoo NF, JBJS 2006;88:480)
- THA = 0.2% (Mahomed NN, JBJS 2003;85A:27).
- Revision THA = 0.95% (Mahomed NN, JBJS 2003;85A:27).
- TSA = <1%
- Most common etiology: S aureus and S epidermidis either by direct contact during arthroplasty or hamatogenous inoculation.
- Increased risk: rheumatoid arthritis, diabetes mellitus, obesity, glucocorticoid use, prolonged surgery, inadequete/poor timing pre-op antibiotics
Periprosthetic Infection Prevention
- Pre-operative antibiotics
- Body exhaust systems
- Laminar flow
- Antibiotic cement
- Prophylaxis for dental/urologic procedures for 2 years following arthroplasty.
Periprosthetic Infection Clinical Evaluation
- Pain (initially at night/rest), fever, chills, draining sinus tracts. Symptoms may be mild and difficult to differentiate between asceptic loosening, instability, etc.
Periprosthetic Infection Diagnositc Tests
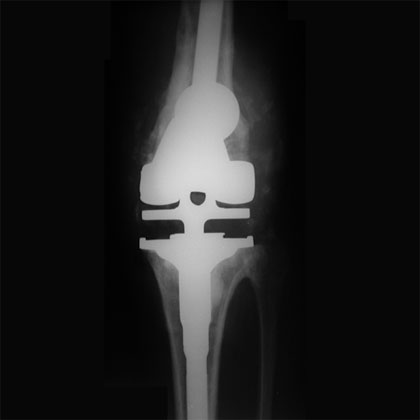
- Xrays: evaluate for periosteal reaction, scattered foci of osteolysis, bone resoprtion, implant wear, progressive radiolucencies, osteopenia, .
- Bone Scan: sensitivity = 33%, specificity = 86%, positive predictive value = 30%, negative predictive value = 88%. (Levitsky KA, J Arthroplasty. 1991;6:237)
- ESR (Westergen erthrocyte sedimentation rate): rises normally after total joint surgery. Returns to normal 6 weeks after surgery. Infection suggested if elevated 3 months after surgery.
- CRP (C-reactive protein): Rises normally after total joint surgery. Returns to normal @3weeks after surgery. Infection suggested if elevated 3 months after surgery. Infection indicated it CRP is higher than 100 mg/L withing 6 weeks of surgery or >10 mg/L for a chronic infection.
- Interleukin-6 (IL-6): Rises normally after total joint surgery. Returns to normal within 48 hours after surgery. Elevated (>10 pg/mL [>10 ng/L]) in patients with periprosthetic infection.
- Aspiration of Joint fluid: send for aerobic culture anaerobic culture, sensitivities, Gram stain, acid-fast staining, CBC with differential. Leukocyte count > 1.7x109/L indicates infection. Infection is likely when knee aspirate contains more than 2500 WBCs per high-powered field (HPF) with >60% neutrophils = Sensitivity of 98% and a specificity of 95% for infection.(Mason JB, J Arthroplasty. 2003 Dec;18(8):1038-43. Erratum in: J Arthroplasty. 2009 Dec;24(8):1293)
- Synovial Leukocyte (WBC) count: 95% and sensitivity of 98% for diagnosing PJI when using a WBC count cut-off value of 2,500 cells/μL combined with a PMN% of > 60. (Mason JB, J Arthroplasty. 2003;18:1038–43). The frequently quoted unit is cells/μL, equivalent to cells/mm3, 106 cells/ L or cells/10-3cm3.
- Leukocyte esterase reagent strips: Moderate or large WBC on strips indicates infection. Sensitivity=92.9%, specificity=88.8%. Blood or debris in synovial fluid renders the strips unreadable in 1/3 of cases. (Parvizi, J, AAHKS annual meeting 2011).
- Acute Infection (within 6 wks of surgery) indicated if: CRP > 100 mg/L, Synovial fluid white blood cell count higher than 10000 cells/µL with more than 90% PMN neutrophils
- Chronic infection indication if: CRP >10 mg/L. Synovial fluid white blood cell count higher than 3000 cells/µL and more than 80% PMN neutrophils.
Periprosthetic Infection Classification / Treatment
-
- Acute (within 4 weeks of arthroplasty, symptoms for < 2weeks): immediate arthrotomy with irrigation and debridement and exchange of polyethylene components and retention of solidly fixed implants followed by 4-6 weeks of IV antibiotics determined by cultures & sensitivities. Failure rate may be 50% with methicillinresistant Staphylococcus aureus (MRSA) infections.
- Late / Hematogenous (>4wks after surgery): Two stage implant exchange. Stage 1: irrigation & debridement with removal of all components and antibiotic cement spacer placement followed by 4-6 weeks of IV antibiotics determined by cultures & sensitivities. TKA Static spacer can be fashion using 2 4.8mm x23cm Steinmann pins rolled with antibiotic cement. One antibiotic covered pin is placed intramedallury in the tibia and one in the femur. Additional cement is placed around the antibiotic cement pins to stabilize the joint and construct (Frank RM, Orthopedics Today Jan 2014). Stage 2: reimplantation with intraoperative cultures.
- Aspiration and culture should be obtained after the patient has been off antibiotics for a minimum of 2 weeks prior to reimplantation.
- Medically unstable: chronic suppressive PO antibiotics.
- Life-threatening sepsis / multiple revisions with severe bone loss and infection: amputation.
- High functional demand patient, young age, loss of extensor mechanism, concomitant soft-tissue reconstruction, immunocompromised patient, resistant organism: arthrodesis.
- Polyarticula rheumatoid arthritis with low function demand: resection arthroplasty.
Periprosthetic Infection Differential Diagnosis
- Loosening
- Osteolysis
- Poly wear
Periprosthetic Infection Complications
- Sepsis
- Functional limitations
Periprosthetic Infection Follow-up Care
Periprosthetic Infection Review References
- Leone JM, JBJS 2005;87A:2335
|