|


|
synonyms:
Os Acromionale ICD-10
- M94.8X1 Other specified disorders cartilage, shoulder
Os Acromionale ICD-9
- 811.01 Fracture of scapula: closed, acromial process
- 726.19 Peripheral enthesopathies and allied syndromes: other specified disorders
- 726.10 Peripheral enthesopathies and allied syndromes: unspecified, RTC syndrome
Os Acromionale Etiology / Epidemiology / Natural History
- Definition = the joining of the acromion to the scapular spine by fibrocartilaginous tissue rather than bone / failure of fusion of the anterior acromial apophysis.
- Incidence = 8%. More common in blacks and males than whites and females. (Sammarco VJ, JBJS 2000;82A:394)
- 1/3 are bilateral
- Generally an asymptomatic finding found on routine xray.
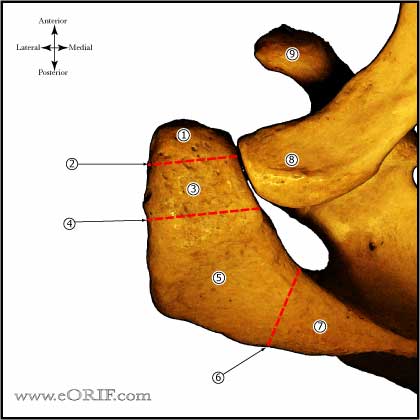
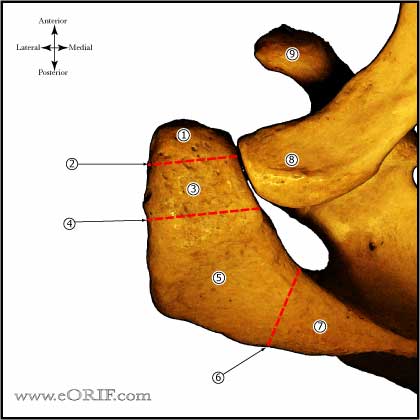
Os Acromionale Anatomy
- Acromial apophysis develops from 4 separate ossification centers: basiacromion, meta-acromion, mesoacromion, and preacromion.
- Complete union of all centers may not occur until age 25.
- The majority of os acromionale occurs between the meta-acromion and mesoacromion.
- Incidence = 8%; 33.3% bilateral; blacks > whites; men > women. (Sammarco VJ, JBJS 2000;82A:394).
Os Acromionale Clinical Evaluation
- Os acromionale is generally asymptomatic.
- Symptomatic = pain with overhead activity, pain when sleeping on affected shoulder, pain is localized to nonunion site.
- Nonunion site is tender.
- May exhibit gross motion at nonunion site.
- May have signs of impingement syndrome.
Os Acromionale Xray / Diagnositc Tests
- A/P, Grashe, Supraspinatus outlet view and axillary views of the shoulder. Os Acromionale is best seen in the axillary view.
- Evaluate supraspinatus outlet view for dynamic impingement with flexion of the anterior fragment.
- MRI:axial cuts best detect os acromionale. Helpful evaluating for other pathology such as RTC tear. Evaluate for reactive changes in the os acromionale site.
- CT: not generally needed, but can clearly dfine lesion on axial cuts.
Os Acromionale Classification / Treatment
- Preacromionale (uncommon): Initial treatment is rest, RTC and periscapular muscle strengthening, ice, modalities, NSAIDS, subacromial injection. Consider corticosteriod injection at the nonunion site. Consider arthroscopic subacromial decompression with fragment excision for very small fragments vs ORIF/bone graft for larger fragments. Arthroscopic excision is done to the superior cortical plate, leaving the deltoid intact. (Wright RW, Arthroscopy 2000;16:595)
- Mesoacromionale (most common): Initial treatment is rest, RTC and periscapular muscle strengthening, ice, modalities, NSAIDS, subacromial injection. Consider corticosteriod injection at the nonunion site. ORIF/bone grafting indicated if non-operative managment fails. Fixation utilizing cannulated screws (Acutrak, Herbert, 4.5mm AO) with/without tension bands placed through the cannulated holes provides improved fixation compared to k-wires. (Warner JBJS 1998;80A:1320)
- Meta-acromionale (rare): Initial treatment is rest, RTC and periscapular muscle strengthening, ice, modalities, NSAIDS, subacromial injection. Consider corticosteriod injection at the nonunion site. ORIF/bone graft indicated if non-operative managment fails.
- Double fragment (preacromial and mesoacromial fragments): Extremely rare, write up a case report.
Os Acromionale ORIF Technique
- (Satterlee CC, JSES 1999;8:125) : (Warner JBJS 1998;80A:1320). (Ortiguera CJ, JSES 2002;11:521).
- Keys: stable fixation and preservation of deltoid and acromial blood supply
- Pre-operative antibiotic
- Anesthesia: GETA, scalene block
- Beach-chair position
- EUA
- Prep and drap
- Perform routine shoulder arthroscopy
- Determine stability of os fragment. If the os is stable standard subacromial decompression is performed.
- After all associated pathology is corrected an incision is made along Langers line over the os lesion. (Hertel R, JSES 1998;7:606)
- The non-union is debrided to bleeding bone on both sides.
- Two guides wires are place retrograde from anterior to posterior in the posterior fragment. The wires are driven out the posterior skin until the wires are flush with the non-union site.
- The fragments are then reduced and compressed with a large tenaculum while the guide-wires are passed into the anterior fragment.
- Place headless compression screws as described by the manufacture.
- Any defect is bone graft (usually from Gerdy's tubercle), small defects can be grafted with demineralized bone graft.
- Consider Figure-of-8 #5 non-absorbable suture placed through the cannulated screws.
- Irrigate
- Close in layers.
- Evaluate subacromial space arthroscopically varifying the anterior acromion is not downslopping.
Os Acromionale Associated Injuries / Differential Diagnosis
- Subacromial impingement: Patients with a stable, asymptomatic os acromionale can be treated with gentle arthroscopic subacromial decompression. The os site should not be violated and the patients should be informed about the risk of the os acromionale as a pain source with the potential need for further surgery to treat it.
- Rotator cuff tear (incidence may be as high as 50%)
- Internal Impingement
Os Acromionale Complications
- Pain-full hardware: generally responds to hardware removal after union occurs.
- Non-union
- Deltoid dysfunction
- Infection
- Pain
Os Acromionale Follow-up Care
- Shoulder immobilizer with pendeulum ROM exercises initially.
- Passive ROM exercises are started at first follow-up appointement (7-10days).
- Shoulder immobilizer is continued for 6weeks, or until bony union is evident radiographically
- Union requires 8-16weeks.
Os Acromionale Review References
- Kurtz CA, JAAOS 2006;14:12
- Burkhart SS, A Cowboy's Guide to Advanced Shoulder Arthroscopy, 2006
- Rockwood and Green's Fractures in Adults 6th ed, 2006
- OKU - Shoulder and Elbow 2nd ed, 2002
- William RC, JSES 2004;13:381
|