|
|
synonyms:calcaneous fracture ORIF, calcaneous fracture fixation, calcaneal fracture open treatment Calcaneous Fracture ORIF Indications
Calcaneous Fracture ORIF Contraindications
Calcaneous Fracture ORIF Alternatives
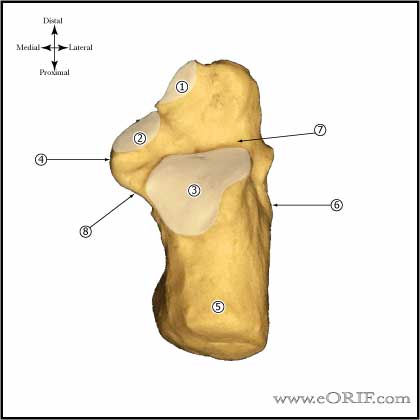
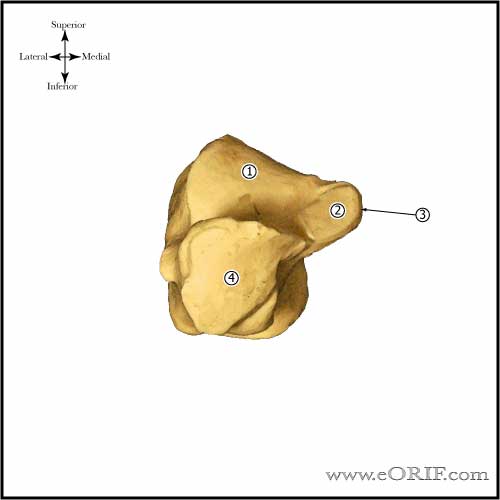
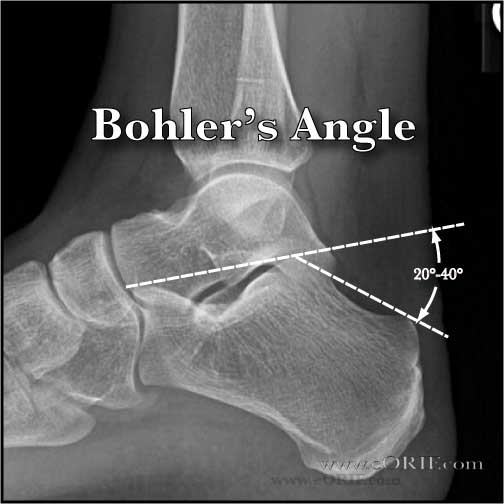
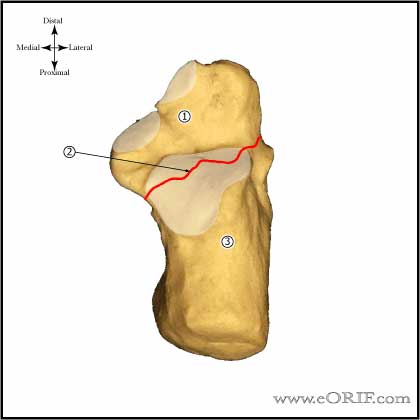
Calcaneous Fracture ORIF Pre-op Planning / Special Considerations
Calcaneous Fracture ORIF Technique
Calcaneous Fracture ORIF Complications
Calcaneous Fracture ORIF Follow-up care
Calcaneous Fracture ORIF Outcomes
Calcaneous Fracture ORIF Review References
|